Fracture Nomenclature for Other Pediatric Carpal Fractures (Non-Scaphoid)
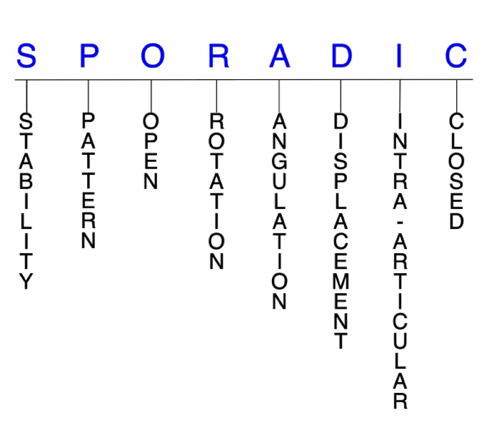
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Other Pediatric Carpal Fractures (Non-Scaphoid), the historical and specifically named fractures include:
Scaphocapitate fracture syndrome
Lunate and perilunate dislocation and fracture-dislocation
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Carpal fractures are rare in the pediatric population. As with adults, fractures of the scaphoid represent the majority of these injuries, accounting for ~0.45% of all upper limb fractures and ~2.9% of all hand and wrist fractures in children. Fractures of the capitate appear to be most common of non-scaphoid carpal fractures, while incidence rates for the other carpals are not well documented due to their low frequency. The rarity of pediatric non-scaphoid carpal fractures is primarily due to the cartilaginous nature of these bones during ossification, as considerable forces are required to injure the unossified or partially ossified carpals. Consequently, multiple carpal fractures are more likely than isolated fractures. Most of these fractures result from forced dorsiflexion wrist injuries—often from a fall on an outstretched hand (FOOSH)—although direct blows causing axial loading of the wrist may also be responsible. A significant number of these injuries are missed upon initial evaluation because plain radiographs often fail to identify them, which is why high clinical suspicion is warranted. Treatment for pediatric non-scaphoid carpal fractures is predominantly conservative and should consist of cast immobilization, while surgery is reserved for displaced fractures and patients approaching skeletal maturity.1-4
Definitions
- A pediatric non-scaphoid carpal fracture is a disruption of the mechanical integrity of one of the non-scaphoid carpals.
- A pediatric non-scaphoid carpal fracture produces a discontinuity in carpal contours that can be complete or incomplete.
- A pediatric non-scaphoid carpal fracture is caused by a direct force that exceeds the breaking point of the bone.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.5-7
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragment’s alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable pediatric non-scaphoid carpal fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
- The incidence of unstable and displaced fractures of the non-scaphoid carpals is less frequent in the pediatric population than in adults because the injury etiology is typically less severe and involves fewer high-velocity mechanisms.8
P - Pattern
- Capitate: head, waist, or body; body fractures may be oblique, transverse, or comminuted9,10
- Generally regarded as second most commonly fractured carpal bone in pediatrics.1
- Typically associated with other injuries—especially scaphoid fractures—and rarely occurs in isolation.11
- The most common mechanism of injury is a FOOSH, with high-energy trauma being necessary to produce scaphocapitate syndrome.12
- Hamate: body or hook of hamate; body fractures may be oblique, transverse, coronal, and/or comminuted
- Body fractures generally result from a FOOSH onto the ulnar border of the hand, while hook fractures are typically due to a direct blow to the ulnar border.
- Body fractures may be associated with injury at the hamate-metacarpal articulation, which often involves an avulsion and displacement at the base of the ring and little metacarpals.1
- Lunate: dorsal pole, volar pole, or body; body fractures may be sagittal, coronal, transverse, and/or comminuted
- Extremely rare, and often fall under the umbrella of perilunate injuries: most are associated with a lunate or perilunate dislocation or fracture-dislocation.1
- Typically result from wrist hyperextension in which the ulnarly-deviated carpus impinges on the distal ulna.13
- Pisiform: proximal pole, distal pole, or body; body fractures may be sagittal, parasagittal, coronal, transverse, and/or comminuted
- Extremely rare, as the pisiform is the last carpal to ossify.1
- Pisiform dislocations appear to be more likely than fractures, and can result from direct trauma on the hypothenar eminence or from an indirect mechanism like lifting a heavy object or a FOOSH.1,14
- Trapezium: trapezial ridge or body; body fractures may be horizontal, vertical, sagittal, coronal, and/or comminuted
- Rare fractures in children.1
- May occur due to axial loading of the adducted thumb and consequent dorsal impaction of trapezial-metacarpal articulation.9
- Trapezoid: dorsal rim or body; may be sagittal, coronal, and/or comminuted
- Rare fractures in children.1
- Usually occur secondary to direct trauma that axially loads a flexed index metacarpal.9
- Triquetrum: dorsal ridge (chip fractures) or body; body fractures may be sagittal, oblique, transverse, and/or comminuted
- High incidence in 11-13-year-olds.
- These injuries rarely occur in isolation.1
- Dorsal chip fractures—which are far more common than body fractures—are often caused by the impact of the ulnar styloid process on the dorsal part of the triquetrum in a FOOSH.3
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of any pediatric non-scaphoid carpal require antibiotics with surgical irrigation and wound debridement but these injuries are extremely rare in children. 5,15,16
- Open fractures of the non-scaphoid carpals may require surgical exploration to determine if articular surfaces are involved. After irrigation and debridement, these wounds are generally left open and further treatment is typically delayed until the wound shows no sign of infection.17,18
- Open pediatric non-scaphoid carpal fractures are also more likely to result in nonunion.19
R - Rotation
- Fracture deformity of any of the pediatric non-scaphoid carpals can be caused by rotation of the bone’s distal fragment on its proximal fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
- Scaphocapitate fracture syndrome consists of concomitant fractures of the scaphoid and capitate with a rotation of 90-180° of the proximal fragment of the capitate. Although possible in children, this injury is extremely rare, and no cases have been documented in which the capitate fragment rotates 180°.20,21
- The pisiform typically moves distally after direct trauma and proximally after indirect mechanisms. It may also rotate significantly after injury, up to a completely inverted position.14
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: fracture line defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
- Very little published information exists concerning the treatment of acute displaced carpal fractures in children.22
- Displacement is another risk factor for nonunion in pediatric carpal fractures.19
- Most pediatric capitate fractures are minimally displaced and therefore only require conservative treatment.1
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- Pediatric non-scaphoid carpal fractures can have fragment involvement with any of their metacarpal, intercarpal, or radial articulations.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.5-7
Pediatric non-scaphoid carpal fractures: named fractures, fractures with eponyms and other special fractures
Scaphocapitate fracture syndrome
- Rare but complex injury that is typically considered a manifestation of the perilunate injury pattern.10,23
- Consists of simultaneous fractures of the scaphoid and capitate neck with a 90-180° rotation of the proximal capitate fragment.21
- Most commonly occurs in young men between ages 20-30, and is very rarely seen and not well documented in children.24,25
- In children, this injury pattern may be associated with other, more obvious fractures.
- It does not appear that any cases of scaphocapitate fracture syndrome have occurred in a child in which the proximal capitate fragment was rotated to 180°.21
- The most recognized mechanism of injury is a volar-applied force to a hyperextended wrist, such as from a fall from a height or vehicular accident.24
- Can be either isolated or associated with a perilunate dislocation, but a substantial force is usually required to cause a dislocation or fracture/dislocation.23
Imaging
- Plain radiographs may not show the extent of the damage to the carpus, in part because the carpal bones may not yet be completely ossified. This, combined with the rarity and complexity of these injuries, may cause the diagnosis to be initially missed or incorrectly labelled as a simple scaphoid fracture.20,2 This is why a high index of clinical suspicion is needed in order to avoid misdiagnosis and ensure appropriate treatment.21,25
- If plain radiography does not lead to a satisfactory diagnosis, a CT scan may be needed, especially if a complex carpal lesion is suspected.20,24
Treatment
- The treatment of this injury pattern is controversial, particularly due to its low incidence.23
- As in adults, conservative treatment—consisting of closed reduction and cast immobilization—may be appropriate for some nondisplaced injuries, but it appears that surgery is often needed in more complex patterns.21,23,25
- Open reduction and internal fixation (ORIF) is generally considered the operative treatment-of-choice in children, particularly for displaced and/or comminuted fractures.
- A dorsal approach is most commonly used, while a volar approach is usually reserved for when decompression of the median nerve is necessary.21,25,26
- K-wires or compression screws are typically recommended to achieve fixation and reduce the risk for nonunion.20,24,25
- According to the literature, it is recommended that reduction of the capitate precedes reduction of the scaphoid.20
Complications
- Infection
- Loss of range opf motion
- Avascular necrosis
- Nonunion
- Carpal bone growth disturbance
Outcomes
- Conservative treatment was found to elicit good outcomes in a small series of children with scaphocapitate fracture syndrome in which the capitate fracture was not displaced.21
- Literature is lacking on outcomes after surgical treatment in pediatrics, but in adults, one study on 15 patients reported that ORIF yielded better results than nonoperative treatment.27
Lunate and perilunate dislocation and fracture-dislocation
- Pediatric dislocations of the lunate are typically divided into perilunate and lunate varieties.28
- Although the two entities should be viewed and addressed separately, it is generally agreed that lunate and perilunate dislocations and fracture-dislocations are different stages of the same injury pattern.28,29
- In lunate dislocations, the lunate is displaced and rotated volarly, while the rest of the carpal bones are in a normal anatomic position in relation to the radius. In perilunate dislocations, the radiolunate articulation is preserved and the rest of the carpus is displaced dorsally.29
- These types of injuries are extremely rare in children, as only a fraction of pediatric carpal injuries involve the perilunate area.30,31
- The mechanism of injury is usually high-energy impact on an outstretched wrist in ulnar deviation, which leads to forced hyperextension.30
- Tran-scaphoid perilunate fracture-dislocations are frequently associated with triquetral fractures.13
Imaging
- Standard wrist posteroanterior (PA) and lateral radiographs are most useful, but a CT scan may be needed if any clinical doubt remains and in order to avoid a delay in diagnosis.
- MRI is effective for identifying intercarpal ligamentous ruptures and occult fractures or bone bruises.29
Treatment
- The optimal management protocol for pediatric lunate and perilunate dislocations and fracture-dislocations is not clearly established because these injuries are so rare. As a result, most treatment recommendations are based on adults.1,30
- In general, it appears that a surgical approach is preferred in most cases over a conservative approach.
- Pure lunate fracture-dislocations can be managed with early closed reduction and percutaneous pinning (CRPP), in which K-wires are used for fixation on any associated fracture(s).30
- Trans-scaphoid perilunate fracture-dislocations can be treated with ORIF through a volar approach.30
- Perilunate dislocations are particularly challenging to manage, and it has been suggested that only surgical treatment can obtain a positive outcome.32
Complications
- Median nerve dysfunction
- Hand or wrist weakness
- Tendon ruptures/dysfunction
- Residual carpal instability
- Infection
- Nonunion
- Malunion
Outcomes
- Although positive outcomes have been identified in several case reports, it’s difficult to determine if the pediatric wrist will eventually return to completely normal finction in the long term.13,30,32
Related Anatomy
- The carpus is composed entirely of cartilage at birth and remains predominantly cartilaginous until late childhood and adolescence. The ossification schedule of these bones affects the likelihood of fracture, fracture pattern, and diagnostic accuracy, depending on the ossification stage.
- The capitate is the first carpal to begin ossification at 1-3 months of age, with the hamate closely following ~1 month later.
- Ossification then proceeds in a clockwise manner, with the triquetrum beginning to ossify between 2-3 years of age, the lunate between 2-4 years, the scaphoid between 4-6 years, and the trapezoid and trapezium around 6 years.2
- The pisiform is the last carpal to ossify, with its center of ossification appearing between 7.5-10 years and usually completing development by age 12. Before this age, the pisiform may be fragmented because of multiple centers.33
- A spherical growth plate circumferentially surrounds the entire ossific center of each carpal during development, which protects the bone and offers resistance to fracture. This continues until a critical bone-to-cartilage ratio is reached at some point in adolescence, at which point carpal fractures start becoming more common. The characteristics of carpal fractures in adolescents approaching skeletal maturity also more closely resemble parallel injuries in adults.9
Incidence and Related injuries/conditions
- Carpal fractures are generally uncommon in the pediatric population, but the scaphoid is by far the most frequently involved of these bones. Scaphoid fractures account for ~0.45% of all upper limb fractures34 and 2.9% of hand and wrist fractures in children.35
- After the scaphoid, the capitate is generally regarded as the next most commonly fractured carpal, although some studies have also identified the triquetrum in this position. Data on incidence rates beyond this are scarce due to the rarity of these injuries.1,4,36
- The incidence of pediatric non-scaphoid carpal fractures increases with age and appears to be highest between ages 11-13, while the occurrence at ≤8 years is far less common.1
Work-up Options
- Pediatric carpal fractures are difficult to diagnose because initial radiographs often fail to reveal the fracture line. Clinicians must therefore have a high index of suspicion when evaluating wrist injuries in children.1
- Routine X-rays
- Usually sufficient for trapezium and triquetrum fractures, with a lateral view being particularly helpful for visualizing dorsal chip fractures of the triquetrum.3
- The key finding on lateral images is a disrupted radius-lunate-capitate axis, while on the PA view, any 1 of the 3 Gilula’s lines can be disrupted.9
- Special radiographic views
- Carpal tunnel and 20° supination oblique views are often required for detecting pediatric hamate fractures.9
- A carpal tunnel view and lateral view of the extended wrist with forearm supination at 30-45° are recommended for diagnosing suspected pisiform fractures and dislocations.14
- For suspected triquetrum fractures, a 45° oblique view is recommended.3
- A Robert or true axial view of the thumb carpometacarpal (CMC) joint may help to supplement routine radiographs for visualizing trapezium fractures.9
- CT scan, MRI, or ultrasound
- May be necessary for suspected fractures not identified on initial radiographs and to visualize associated soft tissue damage.3
Trapezoid fractures are particularly difficult to identify through imaging.9