Fracture Nomenclature for Proximal Humerus fractures
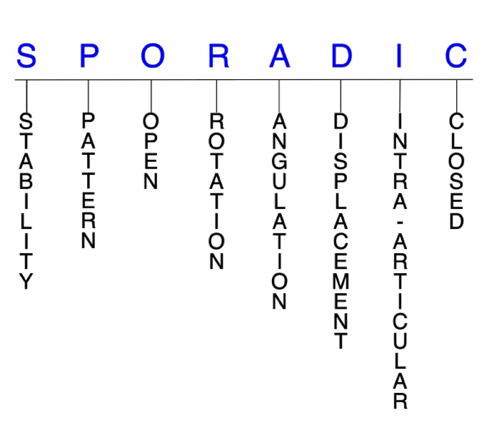
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Proximal Humerus Fractures, the historical and specifically named fractures include no fracture eponyms.
Proximal humerus fractures are very common injuries that occur in a bimodal age distribution. In younger patients, these fractures typically occur secondary to high-energy trauma, such as from a car accident. Proximal humerus fractures are most prevalent in adults over 65 years—particularly women—and the mechanism of injury in this population is usually a low-energy fall that results in a fracture due to the presence of osteoporosis or osteopenia. These fragility fractures in older adults tend to create more complex fracture patterns than those seen in younger patients. Most proximal humerus fractures are nondisplaced or minimally displaced and can therefore be treated conservatively with sling immobilization followed by early, progressive rehabilitation. Surgery may be needed in displaced and more complex fractures, and several options are available.1-4
Definitions
- A proximal humerus fracture is a disruption of the mechanical integrity of the proximal humerus.
- A proximal humerus fracture produces a discontinuity in the proximal humeral contours that can be complete or incomplete.
- A proximal humerus fracture is caused by a direct force that exceeds the breaking point of the bone.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability are not well defined in the literature.5-7
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragments’ alignment is maintained by with immobilization with a sling and/or swathe. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and immobilization. Typical unstable proximal humerus fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
P - Pattern1,8
- Neer classification system
- One-part fracture
- Fracture line involves 1–4 parts.
- None of the parts are displaced (i.e., <1 cm and <45°).
- Two-part fracture
- Fracture line involves 2–4 parts.
- One of these parts (i.e., the greater tuberosity, lesser tuberosity, or articular segment at the anatomic or surgical neck) is displaced (i.e., >1 cm or >45°).
- Three-part fracture
- Fracture line involves 3–4 parts.
- One tuberosity and the surgical neck fracture is displaced; the other tuberosity is attached and results in a rotational deformity.
- Four-part fracture
- Fracture line involves 4 parts.
- All 4 parts (i.e., both tuberosities, the articular surface, and the humeral shaft) are displaced, and the articular portion is usually displaced laterally and out of contact with the glenoid.
- These are typically more severe injuries with a higher risk for complications.
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the proximal humerus require antibiotics with surgical irrigation and wound debridement.5,9,10
R - Rotation
- Proximal humerus fracture deformity can be caused by rotation of the proximal fracture fragment in relation to the distal fracture fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
- In three-part fractures, the nondisplaced tuberosity remains attached, which results in a rotational deformity.8
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angular deformity
- Angulated: bent at the fracture site
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: ≥1 fracture lines defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
- Most proximal humerus fractures (80–85%) are either nondisplaced or minimally displaced and can be treated conservatively. Proximal humerus fractures that are displaced typically involve the surgical neck and may led to long-term functional impairments.3,4
I - Intra-articular involvement
- Intra-articular fractures are those that enter a joint with ≥1 of their fracture lines.
- Proximal humerus fractures can have fragment involvement at the glenohumeral joint.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to post-traumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised, and the risk of post-traumatic osteoarthritis increases significantly.
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.4-6
Related Anatomy1,2,11
- The shoulder is a complex that consists of four joints, with the acromioclavicular and glenohumeral joints being most important for movement. The acromioclavicular joint is a gliding joint formed by the articulation of the acromion and the clavicle. The glenohumeral joint is a ball-and-socket joint formed by the head of the proximal humerus and the glenoid fossa of the scapula.
- The proximal humerus consists of an anatomic neck, the humeral head, the surgical neck, and the greater and lesser tuberosities. The anatomic neck represents the fused epiphyseal plate and lies proximal to the two tuberosities, while the surgical neck is located below the humeral head and is the weakest area of the humerus. The greater tuberosity is the anatomic footprint and insertion point for three of the four rotator cuff muscles, while the lesser tuberosity is the insertion point for the tendon of the subscapularis muscle.
- The humeral head articulates with the shallow glenoid fossa of the scapula, and this articulation allows for complex and dynamic ROM in several planes, making the glenohumeral joint the most mobile of the body.
- Key ligaments of the shoulder include the coracohumeral ligament, which attaches the greater tuberosity to the coracoid process of the scapula, and the superior, middle, and inferior glenohumeral ligaments. These three ligaments form the glenohumeral joint capsule that connects the glenoid fossa to the humerus.
- Key muscles of the shoulder include the pectoralis major, latissimus dorsi, and teres major muscles, as well as the rotator cuff muscle complex, which is comprised of three muscles with tendons that insert onto the greater tuberosity (ie, supraspinatus, infraspinatus, and teres minor) and the large subscapularis tendon, which attaches to the lesser tuberosity.
Incidence
- The overall incidence of proximal humerus fractures is 4–6%, and this figure is expected to continue increasing as the population grows older.1,12
- Proximal humerus fractures are the second most common injuries of the upper extremity and the third most common fracture overall in the population older than 65 years.3
- These injuries are most common in older individuals, and particularly women, who are 2–3 times more likely to experience a proximal humerus fracture than men.1,12