Fracture Nomenclature for Thumb Metacarpal Pediatric Fracture
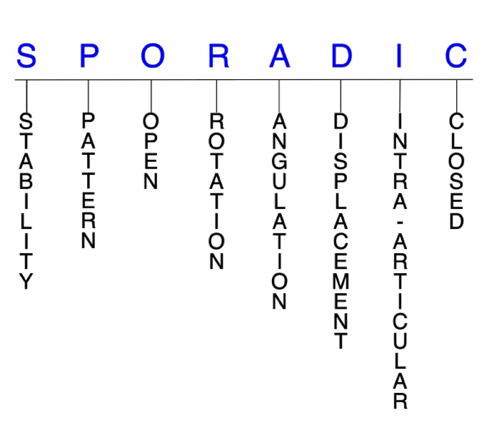
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Thumb Metacarpal Pediatric Fracture, the historical and specifically named fractures include:
Salter-Harris III and IV thumb metacarpal base fracture/Type D fracture
Salter-Harris II metacarpal base fracture/Types B and C fracture
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Fractures of the hand are the most common type of fracture sustained by children, and fractures of the metacarpals account for 10-39% of all pediatric hand fractures. While the incidence of pediatric thumb metacarpal fractures is not well established, some estimates are as high as 21%. Of these, fractures of the thumb metacarpal base are the most common. In children, fractures and fracture-dislocations are more common than true dislocations because the thumb metacarpal bone is weaker than its associated ligaments. Pediatric thumb metacarpal fractures are also less common than their adult counterparts and differ from adult hand fractures owing primarily to the presence of physes. In the growing child, the growth plate is the weakest part of the thumb metacarpal and is frequently involved when this bone is fractured. Most pediatric thumb metacarpal fractures are isolated, simple, closed, and stable injuries, and can be effectively managed conservatively. Surgical intervention may be necessary when closed reduction fails or is likely to fail.1-6
Definitions
- A pediatric thumb metacarpal fracture is a disruption of the mechanical integrity of the thumb metacarpal.
- A pediatric thumb metacarpal fracture produces a discontinuity in the thumb metacarpal contours that can be complete or incomplete.
- A pediatric thumb metacarpal fracture is caused by direct forces that exceed the breaking point of the bone or the epiphyseal plate.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.7-9
- A stable fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragment’s alignment is maintained with simple splinting. Stabile fractures maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put through a partial range of motion (ROM).
- Unstable fractures will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable pediatric thumb metacarpal fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
- The vast majority of pediatric thumb metacarpal fractures are minimally displaced, stable fractures. This is due to the thick periosteal covering and ability of the bone to plastically deform affording a great deal of stability in incomplete fractures.10
- Unlike the phalanges, the metacarpals are relatively protected by their position within the hand and by the stout soft tissues which surround them.1
- Fractures of the border metacarpals generally tend to be less stable and more difficult to control than those of the central metacarpals. Intra-articular metacarpal base fractures are relatively stable.11-1 This stability is primarily due to the osseous architecture of the carpometacarpal (CMC) joints and the interosseous, dorsal and volar CMC ligaments which provide additional stability.13
- In children, even displaced fractures are often easily reduced closed and remain stable following reduction.14
- However, displaced Salter-Harris types III and IV fractures of the pediatric metacarpal thumb are inherently unstable, intra-articular injuries that typically require closed or open treatment to restore the physeal and articular alignment.4,5 Metaphyseal and Salter-Harris II metacarpal base fractures with a radial metaphyseal fragment also tend to be unstable, while Salter-Harris II fractures with an ulnar metaphyseal fragment are typically stable.4
- Similar to two opposing saddles with perpendicular transverse axes, the stability of the thumb CMC joint in power pinch and power grasp motions depends on the joint’s two prime stabilizers. Mechanical instability of this joint is an important factor that may lead to osteoarthritis.15
P - Pattern
- Thumb metacarpal head fractures can occur in oblique, transverse, or comminuted patterns. This type of fracture is rare because the longitudinally directed force that produces them is usually transferred to the proximal metaphysis or thumb CMC joint.11,16 Pediatric thumb metacarpal head fractures are usually epiphyseal, intra-articular injuries that result from direct injury and affect one or both condyles of the metacarpal head, with or without displacement. Interrupting the normal articular surfaces of the metacarpophalangeal (MP) joint increases the chances of arthritis developing if left untreated.5,11,16,17 MP joint effusion and limited motion in the absence of a more obvious metacarpal neck fracture may suggest a pediatric thumb metacarpal head fracture.4
- Thumb metacarpal neck fractures are also rare and tend to result from direct injury. 1,5
- Thumb metacarpal shaft fractures are usually transverse, oblique, spiral, or comminuted, with or without shortening.3 Pediatric thumb metacarpal shaft fractures are more common than those of the head and neck, and are managed similarly to shaft fractures in the other metacarpals.1 These injuries tend to occur in older children, and the pattern usually yields clues to the pathologic forces that caused the fracture, and indicates the mechanism of reduction.1
- Thumb metacarpal base is the most common site of fracture in the pediatric thumb metacarpal. These are typically high-energy injuries that may or may not involve the physis—which is located at the proximal end of the bone near the CMC joint. Pediatric thumb metacarpal base fractures are generally subdivided and managed based on their location, physeal involvement, and intra-articular extension.4,5
- Type A: fractures occurring between the physis and the junction of the proximal and middle thirds of the bone, and the fracture line usually is oriented in a transverse direction or slightly oblique to the shaft. The fracture is often angulated in an apex radial direction and ulnar impaction may be present.1,5
- Type B: Salter-Harris II fractures with a metaphyseal fragment on the ulnar side. These fractures are more common than type C fractures. The shaft fragment is adducted secondary to the adductor pollicis and pulled in a proximal direction by the abductor pollicis longus (APL). This pattern resembles an adult Bennett’s fracture with respect to the deforming forces, but there is no intra-articular extension.1,5
- Type C: Salter-Harris II fractures with a metaphyseal fragment on the lateral side and are less common than type B fractures. Has a reverse pattern, in which the proximal metacarpal shaft is displaced in a medial direction. Often result from substantial trauma and are not reducible by closed manipulation.1,5
- Type D: Salter-Harris III and IV fractures that involve the joint surface and most closely resembles an adult Bennett’s fracture. The deforming forces are similar to the adult Bennett’s and type B fractures with subsequent adduction and proximal migration of the base-shaft fragment, but the intra-articular component of the fracture permits the base-shaft fragment to subluxate laterally at the CMC joint.1,5
O - Open
- A thumb metadcarpal fracture is open when a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of pediatric thumb metacarpal require antibiotics with urgent surgical irrigation and wound debridement.7,18,19
- Open pediatric thumb metacarpal shaft fractures may require an external fixator to prevent shortening and to allow soft tissue healing.11
R - Rotation
- Pediatric thumb metacarpal fracture deformity can be caused by rotation of the distal fragment on the proximal fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
- Oblique and spiral pediatric thumb metacarpal shaft fractures are usually the result of torsional forces and can cause rotational malalignment. These fractures may also angulate or shorten.4,11
- The planes of motion of the thumb are different from those of the rest of the hand. Malrotation is therefore more challenging to judge in the physical examination. The perpendicular relationship of the thumb’s nail plate to those of the other digits provides a good guide. The thumb metacarpal fracture with malrotation is tolerated better than a similar malrotation in the fingers.1
- Unlike the other metacarpals, extra-articular fractures of the thumb metacarpal base can also tolerate moderate malunion in rotation. Example: type A fractures are often angulated in an apex-lateral direction.1,5
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- The surrounding soft tissue attachments and muscles determine the direction of deforming forces for extra- and intra-articular thumb metacarpal fractures. Extra-articular fractures become angulated dorsally owing to extension of the metacarpal base by the APL and flexion of the distal shaft by thenar muscles.20 Salter-Harris II fractures usually have the shaft fragment angulated laterally and slightly proximally from the pull of the APL.1
- Given the large ROM of the thumb, higher degrees of angulation are well tolerated, since the deformity can be compensated for without functional deficit; however, the amount of residual angulation considered acceptable in basilar metacarpal fractures is still a matter of some debate.1,21 Because the motion at the adjacent CMC joint is multiplanar and the fractures are near or involve the physis, the remodeling potential is great. Malangulation ≤20° remodels quite predictably, and even angulation of 30° appears to exhibit significant remodeling, but the improvement in radiographic appearance is less predictable.1
D - Displacement (Contour)
- Displaced thumb metacarpal fracture disrupted cortical contours
- With nondisplaced fractures the fracture line defines one or several fracture fragment fragments; however, the external cortical contours are not significantly disrupted
- In type C fractures, the shaft displacement is ulnarly.1,5
- Isolated thumb CMC joint dislocations almost always displace dorsally, although volar displacement is also possible.22
I - Intra-articular involvement
- Thumb metacarpal intra-articular fractures have a fracture line which enters a joint.
- A pediatric thumb metacarpal fracture can have fragment involvement with its respective MP or CMC joint.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface. Then there is a risk of posttraumatic osteoarthritis.
- Salter-Harris III and IV thumb metacarpal base fractures are intra-articular injuries that are inherently unstable.4
- Differentiating between extra- and intra-articular fractures is crucial for planning an appropriate treatment protocol for pediatric thumb metacarpal fractures. Intra-articular thumb metacarpal base fractures, like those of the little metacarpal base, lack ligamentous support and are therefore prone to subluxation.16
C - Closed
- Closed thumb metacarpal fractures have no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.7-9
Pediatric thumb metacarpal fractures: named fractures, fractures with eponyms, and other special fractures
Salter-Harris III and IV thumb metacarpal base fracture/Type D fracture
- Type D fractures are Salter-Harris III and IV thumb metacarpal base fractures that involve the joint surface.1,5
- These injuries closely resemble the adult Bennett’s fracture, however, whether or not to use eponyms like “children’s Bennett’s fracture” is a matter of debate, with detractors claiming that doing so is unhelpful for establishing management strategies.1,4
- A type D fracture is an inherently unstable, two-part intra-articular avulsion fracture-dislocation. As in adults, the volar oblique ligament holds the volar lip of the epiphysis in place in children.2,4
- The most common mechanism of injury is a fall that axially loads a flexed thumb metacarpal. This causes the thumb metacarpal to dislocate radially and dorsally, taking most of the articular surface with it, and leaving the ulnar "beak" attached to the strong ulnar-volar ligament.2,23
- Supination of the thumb is considered an important element in the mechanism of this injury.23
- An isolated dislocation of the thumb CMC joint without a fracture can also result from a direct blow, but these injuries are extremely rare because the stress transmitted to the joint is mainly dissipated through the adjacent physis of the metacarpal.2,23
Imaging
- In addition to standard radiographic views, Bett’s and Robert’s views are typically required to visualize type D fractures.9
- A Kapandji view can be difficult in pediatric patients because of incomplete ossification of the thumb metacarpal base.15
- Ultrasonography and CT scan are alternative imaging techniques that may occasionally be necessary in certain cases. However, given the higher dose of radiation, CT is not recommended in the pediatric population unless absolutely necessary.11,15
Treatment
- There is some controversy regarding the optimal treatment for these injuries, but most authors agree that the treatment principles are similar to those for adult Bennett’s fractures. Therefore, displaced type D fractures generally require closed or open treatment to restore their physeal and articular alignment because they are unstable.5,23
- Closed reduction and cast immobilization that utilizes longitudinal traction, thumb metacarpal base adduction, and pronation of the thumb ray should be attempted and may be sufficient to achieve fracture reduction.5,23 Direct pressure along the thumb metacarpal base may help push the shaft towards the avulsion component of the fracture.5
- Cast immobilization should then be used for 4-6 weeks and checked by X-ray every week.23
- Closed reduction and percutaneous pin fixation (CRPP) is typically reserved for rare cases in which conservative treatment fails early.5,15,23
- After reduction is verified, percutaneous K-wires are drilled through the thumb metacarpal and into the index metacarpal and/or carpus to hold the position.5
- Percutaneous K-wire fixation can be performed with one transarticular pin or with two intermetacarpal K-wires. Double pinning may prevent rotation and pin breakage.15
- Open reduction and internal fixation (ORIF) is typically required for irreducible type D fractures and/or for recurrent thumb CMC joint dislocation.5,15
- The preferred approach is volar, using a gently curved incision overlying the thumb CMC joint along the glabrous border of the skin.5
- The thumb CMC joint is isolated, opened, and exposed to reveal the articular surface, and provisional reduction is achieved under direct visualization. Subsequently, internal fixation is performed using K-wires or mini-screws. An effort should be made to not cross physis with screw threads as this can disrupt the physis and subsequent growth.1,5
- Additional percutaneous K-wire fixation between the thumb and index metacarpal is often performed to protect the fracture fixation.5
- Ligament repair or reconstruction may also be needed prevent late recurrence of thumb CMC joint dislocation or chronic instability.15
- Whatever the type of treatment for thumb CMC joint reduction, it seems important to combine intermetacarpal or K-wire pinning with 4-6 weeks of immobilization in a gauntlet cast, especially in pediatric trauma cases with restless young patients.15
Complications
- Instability
- First web space contracture
- Pin loosening/pin tract infection
- Nonunion
- Malunion
- Aseptic necrosis
- Stiffening
- Posttraumatic osteoarthritis
Outcomes
- Pediatric patients with thumb CMC joint dislocation treated on the day of injury who demonstrate post-reduction stability have good results after conservative treatment.23
Salter-Harris II metacarpal base fracture/Types B and C fracture
- Types B and C injuries are Salter-Harris II fractures at the thumb metacarpal base.5
- The majority of these injuries are type B, which have a metaphyseal flare on the medial side and the shaft fragment angulated laterally and slightly proximally from the pull of the APL. The adductor pollicis may also adduct the shaft.
- The less common type C injury has the reverse pattern, with the metaphyseal fragment on the lateral side and the shaft displacement medial. This injury may result from more significant trauma and is usually is more difficult to treat by closed methods.1
Imaging
- In addition to standard radiographs, it may be helpful to supplement with a hyperpronated view of the thumb that accentuates the detail at the thumb CMC joint.
- Biplanar views of the thumb are also a must, as type B fractures often appear well reduced in the lateral view of the thumb but are significantly displaced on the anteroposterior (AP) view.1
Treatment
- Simple closed reduction is challenging for types B and C fractures, as the mobility of the metacarpal base and swelling make reduction attempts more problematic. Treatment varies based on the amount of displacement and degree of periosteal disruption.5
- Mild angulation of <20° can be treated by cast application without reduction.
- Moderate angulation is treated with closed reduction and immobilization using a short arm thumb spica splint or cast.
- Repeat radiograph evaluation should be obtained 5-7 days later to check the reduction.5
- Recurrent angulation requires repeat reduction and percutaneous pin fixation, while severe angulation is usually combined with shaft displacement and warrants CRPP.
- CRPP is also preferred if closed reduction is attainable but the reduction is unstable.
- There are multiple options for pin configuration, including direct fixation across the fracture, pinning across the reduced CMC joint, or pinning between the thumb and index metacarpals.5
- Irreducible type B and C fractures typically require ORIF.5
- Type C fractures can be particularly difficult to manage, as they are often more widely displaced and may include a distal fragment buttonholed through the thick periosteum.1 Closed reduction may be attempted for these injuries, but the threshold to progress to ORIF is low, as comminution, soft tissue interposition, or transperiosteal buttonholing may prevent reduction. In these cases, ORIF is performed to extricate the offending structure, followed by pin fixation to maintain alignment.5
Complications
- Post-operative infection
- Intra-articular incongruity
- Pain
- Impaired ROM
- Nonunion
- Malunion
- Aseptic necrosis
- Stiffening
- Instability
- Posttraumatic osteoarthritis
Related Anatomy
- The pediatric thumb metacarpal consists of a distal head that articulates at the MP joint with the proximal phalanx, a supportive neck, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the thumb CMC joint with the trapezium. The thumb CMC joint is a double saddle that is concave in one direction and convex on the other. It moves in flexion/extension, abduction/adduction, and pronation/supination planes, but this greater range of motion results in less inherent stability.20,22,24 In children and adolescents, the physeal plate is located at the proximal end of the thumb metacarpal, which is weaker than the surrounding mature bone. There are also some normal bony variations that may occur:1,4
- A pseudoepiphysis is a persistent expression of the distal epiphysis of the thumb metacarpal, which does not contribute to growth, appears earlier than the proximal epiphysis, and fuses to the metacarpal by age 6 or 7. Pseudoepiphyses are easily be confused with thumb metacarpal fractures, and clinicians therefore must be aware of them.5
- A double epiphysis is an active growth plate present on both ends of the metacarpal. It is usually seen in children with a congenital difference, and its presence does not affect the overall length of the thumb ray. Fractures can occur through a double epiphysis.5
- Ligaments associated with the pediatric thumb metacarpal include the posterior oblique ligament, the dorsal central ligament, the dorsoradial ligament, the first intermetacarpal ligament, and the volar anterior oblique (beak) ligament, which inserts at the thumb metacarpal base and opposes the action of the APL.5,20,24
- Tendons associated with the thumb metacarpal include the APL tendon, which has a broad-based insertion onto the epiphysis and metaphysis of the thumb metacarpal, and the opponens pollicis tendon, which inserts on the anterior and lateral surfaces of the thumb metacarpal shaft.20
Incidence and Related injuries/conditions
- Hand fractures are a common problem in the pediatric population, with a reported incidence of 24.2 hand fractures per 100,000 children each year.17
- Together, metacarpal and phalangeal fractures account for 21% of all pediatric fractures, with the phalanges being fractured more commonly than the metacarpals in this population.2,25
- This distribution is also found in the thumb, as one study found that of 42 thumb fractures, the majority occurred in the proximal phalanx (52%) followed by the metacarpal (31%).26
- Metacarpal fractures account for 10-39% of all pediatric hand fractures.27-30
- The little finger metacarpal is consistently found to be the most commonly injured metacarpal bone, representing 54-80% of these injuries.6,29-31
- According to other studies, the incidence of thumb metacarpal fractures ranges from 4-21%.6,31,32
- In one study on fracture distribution within the thumb metacarpal, of 10 fractures, 80% occurred in the base, 10% in the shaft and 10% in the neck/head.6
- Pediatric metacarpal fractures are most common between ages 13-16, with a median age of 15.29,31 The incidence of thumb fractures in particular increases significantly after the age of 10, and it becomes the second most commonly injured digit after the little finger in adolescence.20 The majority of these pediatric metacarpal fractures (~68%) occur in boys.26 Sports-related injury is the most common mechanism of injury, with most pediatric metacarpal fractures occurring at school (44%) and at the playground or sporting venues (32%).31