Fracture Nomenclature for Index, Long, Ring and Little Metacarpal Fractures Pediatric
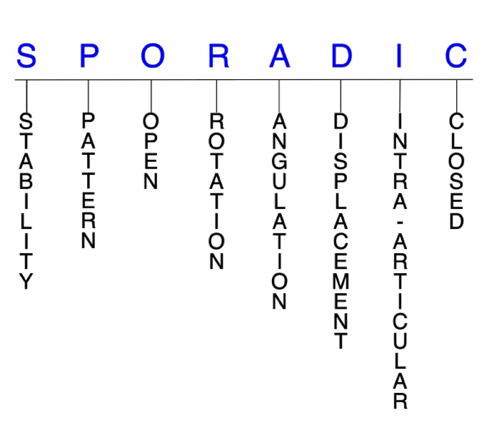
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Index, Long, Ring and Little Metacarpal Fractures Pediatric, the historical and specifically named fractures include:
Index, long, ring, or little metacarpal CMC joint dislocation and fracture-dislocation
Little metacarpal neck fracture/Boxer’s fracture
Epiphyseal and physeal metacarpal fractures
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Fractures of the hand are the most common type of fracture sustained by children, and pediatric metacarpal fractures account for 10-39% of all pediatric hand fractures. Of the metacarpals, the little metacarpal is most commonly fractured and accounts for up to 80% of these injuries. Overall, the little metacarpal neck is the most frequently fractured site in any bone, and the mechanism of injury is typically direct trauma from a blow with a clenched fist against a solid surface. Pediatric metacarpal fractures are also less common than their adult counterparts and differ from adult hand fractures primarily due to the presence of physes. Most pediatric index, long, ring, and little metacarpal fractures are isolated, simple, closed, and stable injuries and can be effectively managed conservatively, but surgical intervention may be necessary when closed reduction fails or is likely to fail.1-4
Definitions
- Pediatric index, long, ring, and little metacarpal fractures are a disruption of the mechanical integrity of these metacarpals.
- Pediatric index, long, ring, and little metacarpal fractures produce a discontinuity in the metacarpal contours that can be complete or incomplete.
- Pediatric index, long, ring, and little metacarpal fractures are caused by direct forces that exceed the breaking point of the bones.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.5-7
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Unstable pediatric index, long, ring, and little metacarpal fractures are rare and typically havesignificant deformity with comminution, displacement, angulation, and/or shortening.
- The vast majority of pediatric metacarpal fractures are minimally displaced, stable fractures, and the thick periosteal covering and ability of the bone to plastically deform afford a great deal of stability in incomplete fractures.8
- Unlike the phalanges, the metacarpals are relatively protected by their position within the hand and the ligaments and other soft tissues that surround them.1
- Fractures of the border metacarpals generally tend to be less stable and more difficult to control than those of the central metacarpals; however, intra-articular metacarpal base fractures are relatively stable.9,10,11 This stability of metacarpal base fractures is primarily due to the osseous architecture of the carpometacarpal (CMC) joints, as the interosseous, dorsal and volar CMC joint ligaments provide stability that resists displacement.11 The base of the index metacarpal is the most stable of the four non-thumb metacarpals, with stability gradually decreasing towards the little metacarpal.11
- In the pediatric population, even most displaced fractures are easily reduced closed and often quite stable.12
P - Pattern
- Metacarpal head: oblique, transverse, or comminuted.
- These rare fractures are usually intra-articular injuries that affect one or both condyles of the metacarpal head, with or without displacement. Interrupting the normal articular surfaces of the metacarpophalangeal (MP) joint will increase the chances of arthritis developing if left untreated.9,13,14
- MP joint effusion and limited motion in the absence of a more obvious metacarpal neck fracture may suggest a metacarpal head fracture.4
- Metacarpal neck: accounting for 56-79% of all pediatric metacarpal fractures, the neck is the most common site of fracture in children.4
- The majority of these occur in the little metacarpal and are also common in the ring metacarpal, while fractures of the index and long metacarpal necks are more rare.1,3
- The mechanism of injury for metacarpal neck fractures often involves a direct blow with a clenched fist on a hard surface. These fractures have a component of axial loading and an element of tangential force. The inherently weaker architecture of the neck fails under these combined forces.1,4
- Closed metacarpal neck fractures are typically angulated with an apex dorsal position due to the deforming force of the interosseous muscles.9,14
- Metacarpal shaft: transverse, oblique, spiral, or comminuted, with or without shortening. Most are spiral in their fracture pattern, which indicates a torsional mechanism of injury, while transverse patterns are less common and represent bending forces.3
- These fractures are relatively rare in children, as they only account for 8-11% of all pediatric metacarpal fractures.4
- The little metacarpal is most commonly affected and accounts for approximately one-half of all pediatric metacarpal shaft fractures.4
- These injuries tend to occur in older children, and the pattern usually yields clues to the pathologic forces that caused the fracture, and indicates the mechanism of reduction.1
- Metacarpal base: account for 10-20% of all pediatric metacarpal fractures, with the majority (72-80%) occurring in the little metacarpal base.4 These fractures can involve the CMC joints, and may be either intra-articular or extra-articular.
- Intra-articular metacarpal base fractures are high-energy injuries associated with CMC joint dislocations, and are uncommon in the index metacarpal, but occur more frequently in the ring and little metacarpal bases.
- Extra-articular base fractures are more common and are usually only minimally displaced due to the stability from the intermetacarpal ligaments.4,14
- In older children, extra-articular fractures typically occur at the metaphyseal-diaphyseal junction and are referred to as “epibasal fractures”, while in skeletally immature children they typically involve the physis, most commonly as a Salter-Harris II fracture.2 Fractures of the ring metacarpal base typically occur with axial loading of this bone with the ring and little CMC joints flexed, causing impaction of the ring metacarpal volar base into the hamate. Fractures through this mechanism are therefore commonly associated with little CMC joint dislocations.11
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk of chronic osteomyelitis. Therefore, all open fractures of the index, long, ring, and little metacarpals require antibiotics with surgical irrigation and wound debridement.5,15,16
- Open fractures to the metacarpal head/neck area, especially those resulting from fistfights, mandate exploration to exclude involvement of the MP joint and/or extensor mechanism. After irrigation and debridement, these wounds are generally left open and internal fixation—if needed—is delayed until the wound shows no sign of infection.9,14 The possibility that these fractures could also be human bites must always be considered.
R - Rotation
- Pediatric index, long, ring, and little metacarpal fracture deformity can be caused by rotation of the distal fragment on the proximal fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
- Oblique and spiral metacarpal shaft fractures are usually the result of torsional forces and can cause rotational malalignment. These fractures may also angulate or shorten.4,9
- In contrast to angulation, rotation is poorly tolerated in metacarpal fractures, as it is magnified with flexion and often results in scissoring of adjacent digits, which interferes with grip.17
- Fragment rotation may be difficult to appreciate, even if a fracture line is identified. Advanced imaging may therefore be necessary in these cases.11
- Even a small amount of rotational malalignment (<10°) of the metacarpals can cause overlap of the digits in flexion and functional disturbance.1
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Most closed pediatric metacarpal neck fractures angulate to an apex dorsal position9,14
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- There is still considerable debate regarding acceptable angulation deformity in metacarpal neck fractures, but most experts agree that more angulation is acceptable in the little and ring than the index and long metacarpals, and that young patients who have remodeling potential can tolerate more angulation.
- Conservative recommendations are that up to 10° of angulation is acceptable in the index, 20° in the long, 30° in the ring, and 40° in the little metacarpal.3,14
- Malunion after a transverse metacarpal shaft fracture can also result in apex dorsal angulation in the sagittal plane, and healing of these fractures may lead to cosmetic and functional complications.14 Dorsal apex angulation of shaft fractures is less tolerated than dorsal apex angulation of neck fractures.
- As the child matures, less angulation can be accepted in the metacarpal neck.1
- The tolerable limit of angulation deformity in the shaft of the index and long metacarpals is <10°, 20° in the ring, and 30° in the little metacarpal.4,17
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: fracture line defining one or several fracture fragment fragments; however, the external cortical contours are not significantly disrupted
- In pediatric metacarpal fractures, the index and little metacarpals are more prone to displace significantly because they only have minimal stabilizing influence from the transverse metacarpal ligaments.1
- Intra-articular fractures of the metacarpal bases occur infrequently. These are high-energy injuries often concomitant with a CMC joint dislocation, and they occur most commonly in the ring and little metacarpals. Some have suggested that intra-articular metacarpal base fractures are underreported and underdiagnosed, due in part to the anatomic structure of the area.11,14 In addition, the overlap of the metacarpal bases on top of each other can make it difficult to visualize dislocation and/or fractures on the lateral wrist or hand x-rays.
- Intra-articular, head-splitting fractures at the metacarpal epiphysis and physis consistent with Salter-Harris fracture patterns seldom occur at the metacarpal level.1
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines are intra-articular.
- Index, long, ring, and little metacarpal fractures can have fragment involvement with their respective MP or CMC joints.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or especially if there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
- Intra-articular incongruity inherently accompanies pediatric metacarpal head fractures.4
- Differentiating between extra- and intra-articular fractures is crucial for planning an appropriate treatment protocol.14
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.5-7
Index, long, ring, and little metacarpal fractures: named fractures, fractures with eponyms, and other special fractures
Index, long, ring, or little metacarpal CMC joint dislocation and fracture-dislocation
- The CMC joints are well protected from injury due to their proximal location in the hand and the stability afforded by the bony congruence and soft tissue restraints, and the ring and little CMC joints are more mobile than those of the index and long metacarpals. For this reason, CMC joint dislocations—with or without a metacarpal base fracture—are rare in children, but they can and do occur.1,3
- Fractures of the metacarpal base or fracture-dislocations at the CMC joint are high-energy injuries with significant tissue disruption, and most of these injuries are transverse in pattern and likely result from axial loading and a flexed metacarpal. A crush injury can also be responsible.1,3
- These injuries are particularly common in the little metacarpal, which has the most mobile CMC joint. This mobility means that intra-articular little metacarpal base fractures can allow subluxation or dislocation of the little CMC joint, which is analogous to a Bennett’s fracture of the thumb.3
- Fractures through the metaphyseal region of the metacarpal base can also occur in pediatrics from a direct blow or axial load, which is often delivered while punching. These are typically small compression injuries that are usually stable.1
- In one large case series on 100 CMC dislocations, >80% of dislocations also involved a fracture, primarily of the metacarpal base or the corresponding carpal bone.18
Imaging
- Radiographic evaluation of metacarpal base and CMC joint injuries may be challenging.
- An adequate lateral view of each digit is required, and because of the transverse arch of the metacarpals, multiple oblique views may also be needed.3
- A CT scan may also be helpful to assess intra-articular metacarpal base fractures or suspected adjacent carpal fractures.3
Treatment
- Displaced extra-articular metacarpal base fractures and CMC joint dislocations can usually be managed nonsurgically with closed reduction.
- Reduction should be accomplished using longitudinal traction combined with a volarly directed pressure on the displaced metacarpal base (in a dorsal CMC joint dislocation) or metacarpal shaft (in a dorsally displaced metacarpal base fracture), followed by cast immobilization.1,3
- Rotational malalignment should be corrected by flexing the MP joint to 90° to tighten the MP collateral ligaments, and then, using the proximal phalanx segment as a rotational lever arm but the fingers should never be cased in this position.3
- If performed correctly, a palpable and audible reduction may accompany a successful manipulation.1
- Unfortunately, most CMC joint dislocations and fracture-dislocations are unstable and casts are usually insufficient for maintaining an anatomic joint reduction. Surgical fixation is therefore needed to maintain reduction in these cases.3,4 Therefore, if a reduction is unstable—which is the rule rather than the exception—closed reduction and percutaneous pinning (CRPP) is strongly recommended.
- Pins can be placed transversely between the metacarpals and through the base of the fractured or dislocated metacarpal, or they can be placed through the collateral recess, across the medullary canal, and across the CMC joint.1
- The lateral pattern is more technically difficult, and care must be taken to avoid the physis. If the medullary canal can be accessed through the collateral recess, the pin can be driven retrograde from distal to proximal, crossing the reduced CMC joint.1
- For isolated little CMC joint dislocations, transverse pins through the metacarpal base into the adjacent metacarpal bases may be adequate, although oblique pins are difficult to introduce, especially in the central rays. Pins are left out of the skin but are protected under a cast or splint, and are then pulled out after 5-6 weeks for dislocations and 4 weeks for unstable fractures. Active and passive ROM exercises are begun with weight bearing activity limitation until full ROM has been achieved.1,3 Open reduction and internal fixation (ORIF) may also be necessary to ensure a stable fixation, and various incisions can be used to gain access to the CMC joint.
- A longitudinal dorsal incision over the involved joint or over the interspace between two adjacent involved joints provides good exposure to the dislocated joint and involved articular surfaces, and will also allow a fasciotomy if necessary.1,3
Complications
- Pain
- Impaired grip strength
- Stiffness
- Malunion
- CMC joint osteoarthritis
- Infection
Outcomes
- In one study on 100 cases of CMC joint dislocations, all patients were treated with either ORIF or CRPP.
- 81% of patients were pain-free and had full ROM at follow-up.18
Little metacarpal neck fracture/Boxer’s fracture
- Little metacarpal neck fractures, commonly referred to as the “boxer’s fracture,” are the most common hand fracture in children, and they account for 41-80% of all pediatric metacarpal fractures.3,19
- These injuries are most commonly observed in the dominant hand of male patients, especially those in the 13-16-year-old age group. Most fractures are nondisplaced or minimally displaced without rotational deformity.1,3,19
- The mechanism of injury is the same as that seen in adult boxer’s fractures, with direct trauma from a blow with a clenched fist against a solid surface most often being responsible, especially in adolescents. Falls and sporting injuries can also lead to this fracture.2,3
- Bending moments at the metacarpal neck can be generated by a force concentrated more dorsally on the epiphysis. These fractures also have a component of axial loading and an element tangential force, and the inherently weaker architecture of the neck fails under these combined forces.1
- Less commonly, a ring metacarpal neck fracture may also occur with the same mechanism of injury.2
Imaging
- Radiographic evaluation of pediatric boxer’s fractures is fairly straightforward, although oblique and lateral views may be most helpful in determining displacement and angulation since the fracture may be subtle with an anteroposterior view.2
Treatment
- Since the majority of pediatric boxer’s fractures are nondisplaced or minimally displaced without rotational deformity, conservative treatment is typically sufficient for these cases.13,19 Conservative treatment generally consists of closed reduction and immobilization in a splint or cast.13
- The plaster forearm-based ulnar gutter splint remains the standard method of immobilization at many medical centers.20 When this is performed, a balance must be struck between immobilizing the extremity long enough to prevent fracture mobility, pain, and nonunion, and allowing movement early enough to avoid stiffness and prolonged rehabilitation.20 The method of immobilization varies according to the splint shape and material, and duration of treatment.20 A number of surgeons have even suggested a more minimalistic approach of functional finger taping or no immobilization at all.20 One potential downside of conservative treatment is that long‑term cast immobilization limits patients’ activities and may lead to a stiff joint and pressure necrosis of the skin, thus prolonging rehabilitation.19
- Surgical intervention may be necessary when the fracture is severely displaced, the angular deformity is substantial, or the finger is rotated causing digital overlap with flexion.13,19 Surgery is also recommended for injuries with a dorsal angulation ≥30˚, a shortening ≥5 mm and rotatory deformity >15˚.19 Percutaneous or cross intramedullary K‑wire fixation is a common procedure used in open reduction for operative treatment, but it has limitations and is associated with complications.19 Other techniques include retrograde pinning by means of intramedullary K-wires, transverse pinning with K-wires, external fixation and standard or low-profile plates, and antegrade intramedullary fixation with a titanium elastic nail.19 Pins are less likely to damage open growth plates than plates and screws in growing children.
Complications
- Reduced grip strength
- Osteomyelitis
- Tendon rupture
- Nerve lesion
- Stiffness
- Pin tract infection
- Pin loosening/migration
Outcomes
- In one study of 69 adolescents aged 12-17 years with a displaced boxer’s fracture, all patients were surgically treated with antegrade intramedullary fixation using a titanium elastic nail. All patients obtained anatomical reduction and presented with complete fracture healing, and there were no cases of complications. Excellent functional results were also presented during the final follow-up at 37 months post surgery. Researchers concluded that this is a straightforward, reliable, minimally invasive surgical technique that seems to achieve excellent functional results.19
- In another study, pediatric patients treated conservatively with a thermoplastic hand-based splint had significantly improved total ROM of the injured digit at 3 weeks compared with those treated with a conventional plaster ulnar gutter splint. At 6 weeks, there was no significant difference, and all patients had adequate ROM by week 12.20
Epiphyseal and physeal metacarpal fractures
- In general, epiphyseal and physeal metacarpal fractures are quite rare, but they are more common in the little metacarpal than any of the other metacarpals. Of the two, injuries to the epiphyses are even more unusual than those of the physes.1,4,21 In one study, physeal fractures only accounted for 18% of metacarpal fractures and 7% of hand fractures overall, and although little metacarpal fractures were most common, extraphyseal metacarpal neck fractures outnumbered physeal fractures 3 to 1.22 One explanation for the low incidence of physeal metacarpal fractures is that the collateral ligaments at the MP joints originate from the metacarpal epiphysis and metaphysis, stabilizing the physis. As a result, metacarpal neck fractures are far more likely to occur than physeal injuries.1,3,4
- Of the physeal fractures that do occur, Salter-Harris II fractures of the little metacarpal appear to be most common, especially in children aged 12-16 years of age.1 One study found that 7% of fractures involved the physis, and 85% of these were Salter-Harris II fractures analogous to metacarpal neck fractures.3
- The mechanism of injury of epiphyseal and physeal fractures is typically a direct dorsal blow to the metacarpal with the MP joint flexed, resulting in an axial load abruptly applied to the distal end of the metacarpal.23
- Although longitudinal growth disturbances have been noted after some metacarpal epiphyseal fractures, the likelihood is probably minimized because most physeal injuries occur in older children.1
Imaging
- Standard posteroanterior, lateral, and oblique views are recommended.
- More advanced imaging studies such as CT scans may be necessary to better visualize pediatric metacarpal head fractures that involve the physis.4
Treatment
- Conservative management may be sufficient for stable and undisplaced epiphyseal and physeal metacarpal fractures. Treatment includes correction of the rotational malalignment followed by reduction of dorsal angulation, with the Jahss maneuver being the preferred method of manipulation. After reduction is maintained, a gutter splint is usually applied with the wrist in neutral, the MP joint flexed to 60°, and the proximal interphalangeal (PIP) joint flexed to ~20°. The joint is immobilized for 3-4 weeks.24
- If the fracture is reducible but unstable, CRPP is recommended. If the metaphyseal fragment is large enough, the wire can gain purchase through it, but the pin must usually cross the physis. In these cases, small diameter smooth wires are recommended, and care must be taken to minimize the number of passes that may further damage the physis.1
- Displaced fractures typically require ORIF. Fixation can consist of smooth wires, screws, or sututres, depending on the size and location of the fragment. Mini-screw fixation for non-physeal injuries is generally preferred over smooth wire fixation for greater stability, although either approach is acceptable.1,3 Immediate aspiration of intra-articular hematoma should also be considered, as it may compromise the physeal and epiphyseal blood supply.1 Although growth arrest is rare, displaced fractures should be followed radiographically until normal growth can be confirmed.3
- If a physeal fracture reduction cannot be accomplished in 1 or 2 attempts, it is better to consider open operative reduction to reduce the chance of growth arrest, which can result in difficult-to-treat angular deformities and joint malalignment due to continued growth in adjacent bones.8
Complications
- Stiffness
- Pain
- Dysfunction
- Infection
- Osteonecrosis
- Growth arrest/disturbance
Outcomes
- ORIF does not guarantee a good result for displaced physeal and epiphyseal fractures, but the ultimate function after these injuries is usually reasonable with this treatment.23
Related Anatomy
Index metacarpal
- The pediatric index metacarpal consists of a distal head that articulates at the MP joint with the proximal phalanx, a supportive neck, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the index CMC joint, primarily with the trapezoid. The base is shaped like a fork, with radial and ulnar condyles that envelop the trapezoid. The radial condyle articulates with the trapezium, while the longer ulnar condyle articulates with the base of the long metacarpal and capitate.25 In developing children and adolescents, the physeal plate is located at the distal end of the index metacarpal, which is weaker than the surrounding mature bone. A pseudoepiphysis can also occur in this bone and may easily be confused with a metacarpal fracture.1,4,45
- Ligamentous attachments include a deep capsular ligament on its volar surface that extends from the trapezium to the base of the index metacarpal, and a superficial ligament. On its dorsal aspect, the base of the index metacarpal has a deep capsular ligament that connects it to the trapezium and a superficial ligament that inserts on the trapezoid. Four strong interosseous ligaments attach the bases of the metacarpals, and the strongest of these is the ligament between the index and long metacarpals.11,26
- The tendons associated with the index metacarpal include the flexor carpi radialis tendon, which inserts onto its volar surface, and the extensor carpi radialis longus (ECRL) tendon, which passes through a dorsal groove on the trapezoid to insert on the radial condyle of the index metacarpal.25,26
- The index CMC joint is an arthrodial diarthrosis, which is inherently stable due to the geometry of its articular surfaces, ligamentous integrity about the joint, and the tethering action of the long extrinsic wrist extensors.27
Long metacarpal
- The pediatric long metacarpal consists of a distal head that articulates at the MP joint with the proximal phalanx, a supportive neck, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the long CMC joint with the distal pole of the capitate and 2 small facets of the index and ring metacarpals. The long metacarpal articulates with the capitate by means of a facet that is concave in its dorsal portion, where it covers the styloid process that projects proximally. This articulation distinguishes the long CMC joint and is considered a keystone due to its more proximal location than the carpal articulations of the other metacarpals.28-30 In developing children and adolescents, the physeal plate is located at the distal end of the long metacarpal, which is weaker than the surrounding mature bone. A pseudoepiphysis can also occur in this bone and may easily be confused with a metacarpal fracture.1,4
- The articulation of the ulnar base of the long metacarpal and the radial base of the ring metacarpal is secured by an interosseous ligament on the volar surface and a CMC ligament on the dorsal surface joins that the long and ring metacarpals to the capitate. There is also a transverse interosseous ligament between the long and index metacarpal, which is the strongest of the intermetacarpal ligaments.1,28
- The primary tendon associated with the long metacarpal is the extensor carpi radialis brevis (ECRB) tendon, which inserts on the dorsoradial aspect of its base, immediately beyond the styloid process. The ECRB has much greater involvement in wrist extension than the ECRL, and it stabilizes the wrist in extension during gripping.11,29
Ring metacarpal
- The ring metacarpal consists of a distal head that articulates at the MP joint with the proximal phalanx, a supportive neck, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the ring CMC joint with the long metacarpal, little metacarpal, capitate, and hamate. The quadrilateral base is small and considerably variable, with 5 different morphologies. It can either articulate solely with the radial half of the hamate articular surface or it can articulate with both the hamate and the capitate through a smaller radial facet.11 In developing children and adolescents, the physeal plate is located at the distal end of the ring metacarpal, which is weaker than the surrounding mature bone. A pseudoepiphysis can also occur in this bone and may easily be confused with a metacarpal fracture.1,4
- Ligaments associated with the ring metacarpal include an interosseous ligament on the volar surface and a CMC ligament on the dorsal surface.11
- The ring metacarpal is the only metacarpal that does not have any proximal tendon attachments to act as a deforming force when a fracture occurs. This is one of the main reasons that reports of isolated fractures of the ring metacarpal base are essentially nonexistent in the literature.11,17
- The ring CMC joint has far greater ROM than the index and long CMC joints. It allows marked flexion-extension of up to 20°, radial-ulnar deviation of up to 7°, and pronation-supination of up to 27°. The motion of the ring CMC joint also must be intact to afford the full ROM to the very mobile little CMC joint, and its motion in all 3 directions is paramount for grasping and palmar cupping in normal hand functioning.11
Little metacarpal
- The little metacarpal consists of a distal head that articulates at the MP joint with the proximal phalanx, a supportive neck, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the little CMC joint with the ring metacarpal and the hamate. The proximal surface of its base is a facet that is concave from side to side and convex from its volar to dorsal aspect, for articulation with the hamate. Its lateral aspect features an elongated strip-like facet for articulation with the ring metacarpal.31,32
- In developing children and adolescents, the physeal plate is located at the distal end of the little metacarpal, which is weaker than the surrounding mature bone. A pseudoepiphysis can also occur in this bone and may easily be confused with a metacarpal fracture.1,4
- Ligamentous attachments of the little metacarpal include the pisometacarpal ligament, which is a distal extension of the flexor carpi ulnaris (FCU) that attaches to the base of the little metacarpal, the deep transverse metacarpal ligament, natatory ligament, an interosseous ligament and the dorsal CMC ligament that attaches to the hamate.32
- The tendons associated with the little metacarpal include the extensor carpi ulnaris (ECU) tendon, which passes through the ECU groove of the ulna and inserts at the dorsalulnar aspect of the base of the little metacarpal, and the FCU tendon. The ECU functions not only as the ulnar wrist extensor and ulnar deviator, but also as the dynamic stabilizer of the distal radio-ulnar joint.32
- The shallow saddle-shaped bony configuration of the little CMC joint provides intrinsic stability but allows an average of 30° flexion-extension.31
Incidence and Related injuries/conditions
- Hand fractures are a common problem in the pediatric population, with a reported incidence of 24.2 hand fractures per 100,000 children each year.13 Together, metacarpal and phalangeal fractures account for 21% of all pediatric fractures, with the phalanges being fractured more commonly than the metacarpals in this population.2,33
- Metacarpal fractures account for to 10-39% of all pediatric hand fractures.22,34-36 The little finger metacarpal is consistently found to be the most commonly injured metacarpal bone, representing 54-80% of these injuries.35-38 Incidence rates range from 4-21% in the thumb metacarpal, 4-6% in the index metacarpal, 1-19% in the middle metacarpal, and 4-17% in the ring metacarpal.37-39
- Metacarpal base fractures account for 10-20% of all pediatric metacarpal fractures, and the little metacarpal is most commonly involved, accounting for 72-80% of pediatric metacarpal base fractures.3,35,38
- Metacarpal shaft fractures are relatively uncommon and only account for 8-11% of all pediatric metacarpal fractures. The little metacarpal is most commonly involved, representing approximately 50% of all reported pediatric metacarpal shaft fractures.35,38
- The metacarpal neck is the most common site of fracture in this bone, as they account for 56-79% of all pediatric metacarpal fractures. The little metacarpal is most commonly involved, accounting for 60-67% of all pediatric metacarpal neck fractures.35,38
- Pediatric metacarpal fractures are most common between ages 13-16, with a median age of 15. The highest incidence of fracture in this age group is little metacarpal neck fractures.35,37
- The majority of these injuries—approximately 68%—occur in boys.35,37
- Sports-related injury is the most common mechanism of injury, with most pediatric metacarpal fractures occurring at school (44%) and at the playground or sporting venues (32%).37
- In one study, ball games were found to be the single most common cause of hand fractures in both genders, but in 13-16 year-olds, fractures caused by punching were more common, although nearly exclusive to boys.22