Fracture Nomenclature for Thumb Metacarpal Fractures
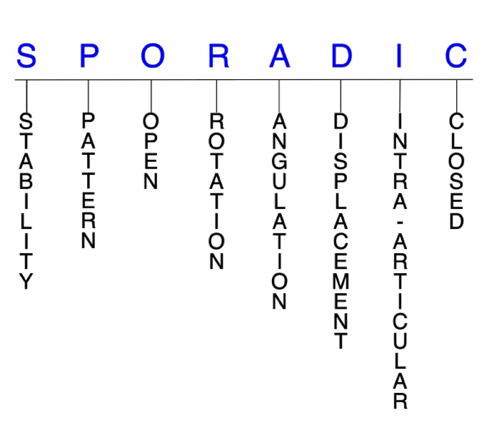
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Thumb Metacarpal Fractures, the historical and specifically named fractures include:
Bennett's Fracture
Rolando's Fracture
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Metacarpal fractures represent some of the most common injuries seen in emergency departments. Metacarpal fractures account for 18-44% of all hand fractures, and the little metacarpal is the most frequently affected. Fractures of the thumb metacarpal rank second in prevalence, representing 12-25% of all metacarpal fractures. Bennett’s fractures and Rolando’s fractures are two of the most typical fracture patterns seen in the thumb metacarpal. These injuries typically result from an axial load on the thumb with a clenched fist or the thumb abducted or extended. Most thumb metacarpal fractures can be treated similarly to fractures of other metacarpals, and a variety of conservative and surgical options are available. However, some unique features of the thumb must be taken into consideration when determining treatment to prevent long-term complications and impaired hand function.1-6
Definitions
- Thumb metacarpal fractures are a disruption of the mechanical integrity of the thumb metacarpal.
- Thumb metacarpal fractures produce a discontinuity in the thumb metacarpal contours that can be complete or incomplete.
- Thumb metacarpal fractures are caused by direct forces that exceed the breaking point of the bone.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.7-9
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragment’s alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: fracture fragment will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable thumb metacarpal fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
- Fractures of the thumb metacarpal base are inherently unstable, and appropriate treatment is necessary to avoid complications like osteoarthritis, weakness, and loss of thumb carpometacarpal (CMC) joint function.10,11
P - Pattern
- Thumb metacarpal head: oblique, transverse, or comminuted, these fractures are uncommon because the longitudinally directed force that produces them is usually dissipated at the proximal metaphysis or thumb CMC joint; they can also involve the metacarpophalangeal (MP) joint.1,2
- Thumb metacarpal neck: this fracture pattern is possible but extremely rare.
- Thumb metacarpal shaft: transverse, oblique, or comminuted, with or without shortening; each fracture type presents characteristic deformities that may lead to complications if unrecognized or not managed appropriately.1,2
- Rare fracture pattern: due to the absence of firm fixation of the proximal portion of the metacarpal, force directed to the shaft is often transferred to the base and results in a fracture at that location.12
- Comminuted thumb metacarpal shaft fractures are usually the result of direct trauma and are often associated with soft tissue injury.1
- Thumb metacarpal base: by far the most common site of fracture in the thumb metacarpal, they can involve the thumb CMC joint, and may be either intra-articular or extra-articular.
- Intra-articular base fractures are high-energy injuries typically associated with thumb CMC joint dislocation or subluxation.2
- Extra-articular fractures are usually transverse or mildly oblique. They generally occur at the proximal metaphyseal-diaphyseal junction and are referred to as epibasal fractures.1
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk of developing osteomyelitis. Therefore, open fractures of the thumb metacarpal require antibiotics with surgical irrigation and wound debridement.7,13,14
- Open thumb metacarpal shaft fractures may require an external fixator to prevent shortening and to allow soft tissue healing.1
R - Rotation
- Thumb metacarpal fracture deformity can be caused by rotation of the distal fragment on the proximal fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
- Oblique and spiral thumb metacarpal shaft fractures are usually the result of torsional forces and can cause rotational malalignment. These fractures may also angulate or shorten.
- Unlike other metacarpals, extra-articular fractures of the thumb metacarpal base can tolerate moderate malunion in rotation.1
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- Example: thumb metacarpal shaft fractures are often angulated with its apex dorsal such that the distal fragment is adducted and flexed.1
- Given the large ROM of the thumb, higher degrees of angulation are well tolerated, as the deformity can be compensated for without functional deficit.15
- The surrounding soft tissue attachments determine the direction deforming forces for both extra- and intra-articular thumb metacarpal fractures. Extra-articular fractures become angulated dorsally owing to extension of the metacarpal base by the abductor pollicis longus (APL) and flexion of the distal shaft by thenar muscles.
- Apex dorsal angulation up to 30° is acceptable for extra-articular thumb metacarpal base fractures, but angulation beyond this limit will narrow the thumb web space and cause compensatory MP joint hyperextension, which is poorly tolerated.6
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: fracture line defining one or several fracture fragment fragments; however, the external cortical contours are not significantly disrupted
- In Bennett’s fractures, the anterior oblique, or beak ligament prevents displacement of the volar fragment, but the dorsal fragment displaces via the APL with the shaft displaced by the extensor pollicis longus (EPL) and adductor pollicis6, resulting in shortening and joint subluxation.
- Isolated thumb CMC joint dislocations almost always displace dorsally, although volar displacement is also possible.16
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- Thumb metacarpal fractures can have fragment involvement with its MP or CMC joint.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
- Differentiating between extra- and intra-articular fractures is crucial for planning an appropriate treatment protocol for thumb metacarpal fractures.2
- Intra-articular thumb metacarpal base fractures, like those of the little metacarpal base, lack ligamentous support and are prone to subluxation.2
- The majority of intra-articular thumb metacarpal base fractures are described as either Bennett’s or Rolando’s fractures, and they present treatment challenges secondary to the deforming forces acting at the base of the thumb.17
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.7-9
Thumb metacarpal fractures: named fractures, fractures with eponyms, and other special fractures
Bennett’s fracture
- Intra-articular avulsion fracture of the thumb metacarpal base that consists of a single, variable-sized, volar-ulnar fracture fragment and results in subluxation or dislocation of the thumb CMC joint.1,10
- These fractures account for about one-third of all thumb metacarpal fractures in adults and are inherently unstable.10
- Occur when the thumb metacarpal is axially loaded and partially flexed, and most are caused by indirect forces such as falling on an extended or abducted thumb or an impact onto a clenched fist.1,10
- This force can result from punching injuries in which a flexed and adducted thumb strikes the opponent’s head or jaw, but the incidence from falls, motor vehicle accidents, and work injuries appears to be similar.10
- Adult males are most likely to experience this injury, and it usually occurs in the dominant hand.10
- The resultant avulsed volar-ulnar fragment of the metacarpal base is of variable size and pyramidal in shape, and it is held to the trapezium by the anterior oblique ligament. The metacarpal shaft is then pulled radially, proximally, and dorsally by the APL, EPL, extensor pollicis brevis (EPB), and adductor pollicis, and the remaining metacarpal base subluxates in these directions, which can lead to complete dislocation.1,2,6
- Isolated thumb CMC joint dislocation without associated fracture is a very rare injury that accounts for <1% of all hand injuries. Some refer to this injury as a "Bennett’s fracture without the fracture."
- These injuries almost always displace dorsally—although there are reports of volar dislocation—and are classified as simple or complex.
- The mechanism of injury is axial loading and flexion of the thumb metacarpal. This force causes flexion and axial loading of the metacarpal base, and results in dorsolateral ligament rupture and dorsal subluxation.16
Imaging
- In addition to lateral radiographic views, Bett’s and Robert’s views are typically required to visualize the injury.1
- CT scan is typically unnecessary, but may be used if comminution is suspected.1 (It is also helpful in determining the size and positino of the volar ulnar fracture fragment.)
Treatment
- Several options are available for treating Bennett’s fractures, but a consensus has not yet been reached on the best technique. There are advocates for both conservative and surgical approaches, and each comes with associated advantages and disadvantages.1,10
- Closed reduction methods involve traction on the thumb to pull the metacarpal distally with concurrent gentle pressure pushing the metacarpal base medially to return it to anatomical position.
- Because these fractures are unstable, the primary goal is to obtain and maintain adequate reduction to allow healing in an anatomical position, as failure to do so can lead to long-term consequences like osteoarthritis, weakness, or loss of thumb CMC joint function.10
- The most basic method is reduction under adequate analgesia followed by plaster cast immobilisation for up to 6 weeks with the thumb in a position of moderate adduction and opposition 10 however, due to fracture instability, redisplacement is common.
- Closed reduction and percutaneous pinning (CRPP) typically involves reduction followed by percutaneous insertion of a K-wire through the base of the metacarpal across the joint and into the fracture fragmentto hold the reduction in place. The wire remains in place for ~4-6 weeks and removal is followed by rehabilitation.10
- The K-wire can also be fixated between the thumb and index metacarpals with intermetacarpal pinning.1
- An alternative approach places the K-wire into the distal metacarpal fragment and then applies traction on the wire via a frame and rubber bands to reduce the fracture and maintain this position.10
- CRPP is generally considered the preferred method of treatment for small Bennett’s fractures when: the fragment is <15-20% of the articular surface, there is <3 mm of displacement, and the concave dome is maintained.1,2
- Bennett’s fractures that involve >25% of the joint surface, with >3 mm displacement, and irreducible by closed techniques should treated with open reduction and internal fixation (ORIF).2
- A Wagner incision is recommended, and either K-wires or lag screws may be used to hold the reduction in place.1,10
- If pins are used, the thumb should be postoperatively immobilized in a thumb spica cast for up to 4 weeks, and the transarticular pin is removed. The pins holding the fracture fragment are removed at 6 weeks.
- Screw fixation, although technically more demanding, is more secure, and active ROM may be initiated 5-10 days postoperatively.1
- Arthroscopic reduction and fixation is another option for any Bennett’s fracture that necessitates surgery, but this approach is not recommended for complex articular fractures that are not amenable to percutaneous pinning or screw fixation. Chronic injuries requiring osteotomy and reduction may also require open treatment.
- About 7-10 days after the procedure, the sutures are removed and a thermoplastic forearm-based thumb spica splint is fabricated for the patient with the thumb interphalangeal (IP) joint left free.
- A plaster splint or cast may be necessary if the patient is unable to cooperate with restrictions.
- Percutaneous pins are usually removed at 4-6 weeks, and gentle motion of the thumb is allowed at 4-6 weeks if the examination warrants it. Full motion of the index, long, ring, and little fingers are encouraged immediately after surgery.18
- Debate exists regarding the optimal management for isolated thumb CMC joint dislocations; options include closed reduction and casting, percutaneous fixation, ligamentous repair or reconstruction, and capsular placation followed by K-wire fixation ligament reconstruction.
- If the joint is stable, closed reduction and a plaster cast with the thumb in abduction for 4-6 weeks is the preferred treatment.
- If the joint is unstable, it is preferable to hold the reduction with K wires, with or without capsulorrhaphy16 or ligament reconstruction.
Complications
- Instability
- First web space contracture
- Pin tract infection
- Pin loosening
- Malunion
- Nonunion
- Stiffening
- Posttraumatic osteoarthritis
- Complex regional pain syndrome (CRPS)
Outcomes
- Studies generally suggest that ORIF for Bennett’s fractures is associated with more reliable reduction and better long-term outcomes that other approaches, but the technique is technically demanding.10
- One study evaluated patients nearly 10 years after conservative management of Bennett’s fractures and noted little evidence of symptomatic arthritis despite imperfect reduction.19 Another study noted a higher incidence of symptomatic arthritis when articular incongruity persisted after reduction.20
- Some experts claim that there is no significant difference in clinical outcomes between ORIF and CRPP, as long as anatomic alignment is achieved. Long-term degenerative changes may also become evident radiographically after these interventions.1
- Conservative management using a spica cast elicited equally good outcomes for isolated thumb CMC joint dislocations compared to various ligamentous reconstructive procedures. However, recurrent instability is a concern, and ligament reconstruction should be considered in unstable cases.16
- ORIF combined with an early, active rehabilitation program led to satisfactory functional and radiological outcomes in treating Bennett’s fractures, and are considered an efficient option.11
- In a study that compared arthroscopically assisted screw fixation to ORIF, there were fewer complications, shorter immobilization time, and diminished tourniquet time in the former versus the latter group.21
Rolando's fracture
- Rolando’s fractures are comminuted intra-articular fractures of the thumb metacarpal base that may have a Y- or T-type fracture pattern.15
- Rolando’s fractures are less prevalent than Bennett’s fractures, but the deforming forces involved are the same.
- First described in 1910 as a Y-shaped pattern with 3 major segments: metacarpal shaft, volar fragment, and dorsal fragment. However, the term has come to mean all intra-articular thumb metacarpal base fractures with ≥3 segments, and highly comminuted fractures are often placed in this category.17
- Often caused by an axial load crushing the articular surface. The base is usually split into a volar and dorsal fragment, with the volar oblique ligament attached to the volar segment and the shaft pulled proximally and dorsally, primarily by the APL and the adductor pollicis.17
Imaging
- Because Rolando’s fractures can appear deceptively benign on plain radiographs, a CT scan may be needed to assess the comminution and extent of articular disruption.1
Treatment
- In general, treatment options available for Rolando’s fractures are similar to those for Bennett’s fractures, but surgical management appears to be preferable over conservative management, especially for unstable fractures.15,17
- For classic three-part Rolando’s fractures when there are large dorsal and volar fragments, ORIF with either multiple K-wires or a plate is recommended, but this approach may be unproductive if there is significant comminution.1,17
- The surgical exposure for plate fixation is the same as for Bennett’s fractures: longitudinal traction is applied, and a provisional reduction of the two articular fragments is held with K-wires, a reduction clamp, or both.1
- Neurovascular damage is a major complication of this approach, and care should be taken not to damage the branches of the superficial radial nerve, the lateral antebrachial cutaneous nerve, or the radial artery.17
- A bone graft may also be needed if there is a metaphyseal void secondary to compaction of the cancellous subchondral bone.1
- In the absence of large volar and dorsal fragments, closed reduction with external fixation is indicated. Several options are available, including CRPP with K-wires. To achieve reduction, the thumb is abducted and pronated, and longitudinal traction is applied.17
- Successful CRPP is usually difficult to accomplish in Rolando’s fractures because of the difficulty involved in reducing all the articular fragments. Articular reduction is most likely to be successful when there are two fragments with minimal comminution.1
- If there is persistent pain after surgery, patients should not be treated for ≥6 months. If pain persists, or there is radiographic evidence of articular incongruity, arthrodesis of the thumb CMC joint is recommended.1
Complications
- Stiffness
- Infection
- Neurovascular damage
- Posttraumatic osteoarthritis
- Malunion
- Nonunion
Outcomes
- Rolando’s fractures are typically associated with a poorer prognosis than Bennett’s fracture, primarily due to its comminuted nature.
- Studies have shown decreased palmar abduction, key pinch strength, and impairment scores in patients with Rolando’s fractures versus Bennett’s fractures.
- Exact anatomic reduction of the articular surface may not be necessary to obtain a good functional result; however, reduction to ≤1 mm is thought to reduce the risk of arthritis.17
- The best prognosis is for the classic 3-part Rolando’s fractures in which the volar-ulnar and dorsal articular fragments can be anatomically reduced and stabilized. For more comminuted fractures, anatomic reduction is more challenging or may be impossible, making distraction and external fixation more appropriate.15
Related Anatomy
- The thumb metacarpal consists of a distal head that articulates at the MP joint with the proximal phalanx, a supportive neck, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the thumb CMC joint with the trapezium. The thumb CMC joint is a double saddle that is concave in one direction and convex on the other. It moves in flexion/extension, abduction/adduction, and pronation/supination planes, but this greater ROM results in less inherent stability.6,10,16
- Ligaments associated with the thumb metacarpal include the posterior oblique ligament, the dorsal central ligament, the dorsoradial ligament, the first intermetacarpal ligament, and the volar beak (anterior oblique) ligament, which inserts at the thumb metacarpal base and opposes the action of the APL.6,10
- Tendons associated with the thumb metacarpal include the APL tendon, which inserts onto the base of the volar side of the thumb metacarpal base, and the opponens pollicis tendon, which inserts on the anterior and lateral surfaces of the thumb metacarpal shaft.6
- The biconcave structure of the thumb CMC joint has been reported to provide as much as 47% of the joint stability while in opposition.6
Incidence and Related injuries/conditions
- Metacarpal and phalangeal fractures account for nearly half of all hand injuries that present to the emergency room.22
- Metacarpal fractures are less common than phalangeal fractures, but comprise between 18-44% of all hand fractures.23,24
- It is estimated that >250,000 metacarpal fractures occur in the U.S. each year.23
- An overall incidence rate of 13.7 metacarpal fractures per 100,000 person-years has been reported, with these injuries comprising 33% of all hand fractures in the U.S.3
- Thumb metacarpal fractures account for ~12-25% of all metacarpal fractures, which places them second only to little metacarpal fractures in terms of prevalence.6,23
- Of all thumb metacarpal fractures, >80% involve the base.6