Fracture Nomenclature for Little Metacarpal Fractures
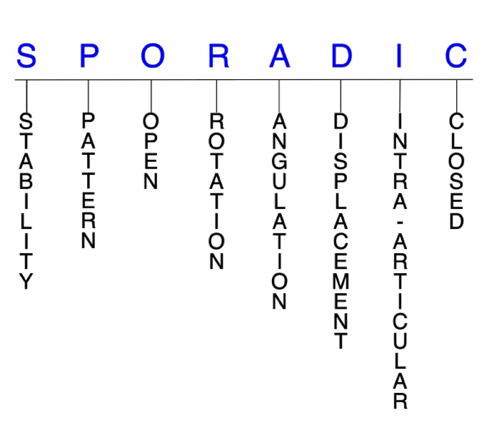
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Little Metacarpal, the historical and specifically named fractures include:
Little metacarpal neck fracture/Boxer’s fracture
Little CMC joint fracture-dislocation/Reverse Bennet’s fracture
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Fractures of the metacarpals occur less frequently than phalangeal fractures, but still represent some of the most common injuries seen in emergency departments. Reports suggest that metacarpal fractures comprise as much as 44% of all hand fractures, and the little metacarpal is the most frequently affected of these bones. Little metacarpal fractures account for approximately 11% of all hand fractures. Little metacarpal fractures are primarily seen in young and active adults, and the typical injury mechanism is an axial force to the knuckle of a closed fist with a concomitant bending moment, which is usually the result of a punching injury or—less commonly—a fall. Although there is still some debate regarding the optimal treatment strategy for certain little metacarpal fractures, most of these injuries are isolated, closed, and stable, and can therefore be managed effectively with a conservative approach. Surgery, however, may be necessary when conservative treatment fails to reduce the fracture or is likely to fail.1-6
Definitions
- Little metacarpal fractures are a disruption of the mechanical integrity of the little metacarpal.
- Little metacarpal fractures produce a discontinuity in the little metacarpal contours that can be complete or incomplete.
- Little metacarpal fractures are caused by direct forces that exceed the breaking point of the bone.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.7-9
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragment’s alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable little metacarpal fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
- The base of the little metacarpal is the least stable of the non-thumb metacarpals, with stability gradually increasing towards the index metacarpal base. Little metacarpal base fractures and little carpometacarpal (CMC) joint fracture-dislocations therefore tend to be unstable.11
P - Pattern
- Little metacarpal head: oblique, transverse, or comminuted. Comminuted fractures are most common at this location.
- Can involve the metacarpophalangeal (MP) joint.
- These are usually intra-articular fractures that affect one or both condyles of the metacarpal head, with or without displacement. Displaced fractures can affect joint congruity.1,2
- Little metacarpal neck: most common site of fracture in all metacarpals, with the highest incidence in the little metacarpal; closed metacarpal neck fractures are typically angulated to an apex dorsal position due to the deforming force of the interosseous muscles.1,2
- These fractures typically result from direct axial force, causing failure of the volar cortex and flexion deformity.12
- Little metacarpal shaft: transverse, oblique, or comminuted with or without shortening. Each fracture type presents characteristic deformities that may lead to complications if unrecognized or not managed appropriately.1,2
- Fractures of the little metacarpal shaft rank behind the neck in incidence and can cause cosmetic deformity if significant malunion occurs.13
- Little metacarpal base: can involve the little CMC joint, and may be either intra-articular or extra-articular; intra-articular metacarpal base fractures are high-energy injuries associated with CMC joint dislocation, and are fairly common in the little metacarpal; most extra-articular base fractures are only minimally displaced due to stability from the intermetacarpal ligaments.2
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for osteomyelitis. Therefore, open fractures of the little metacarpal require antibiotics with surgical irrigation and wound debridement.7,14,15
- Open fractures in the little metacarpal head/neck area—especially those resulting from fistfights—mandate exploration to exclude involvement of the MP joint and/or extensor mechanism. After irrigation and debridement, these wounds are generally left open and internal fixation—if needed—is delayed until the wound shows no sign of infection.1,2
R - Rotation
- Little metacarpal fracture deformity can be caused by rotation of the distal fragment on the proximal fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
- Oblique and spiral little metacarpal shaft fractures are usually the result of torsional forces and can cause rotational malalignment. These fractures may also angulate or shorten.1
- In contrast to angulation, rotation is poorly tolerated in little metacarpal fractures, as it is magnified with flexion and often results in scissoring, which interferes with grip.4
- Example: most closed little metacarpal neck fractures angulate to an apex dorsal position.1,2
- Fragment rotation may be difficult to appreciate, even if a fracture line is identified. Advanced imaging may therefore be necessary in these cases.11
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- The tolerable limit of angulation deformity in the little metacarpal neck varies from as low as 40° to as high as 70°.2
- In significantly angulated boxer’s fractures of the little metacarpal neck, “pseudo-clawing” may be observed due to altered mechanics of the extensor apparatus.16
- Malunion after a transverse metacarpal shaft fracture can also result in apex dorsal angulation in the sagittal plane, and healing of these fractures may lead to cosmetic and functional complications. 2
- The tolerable limit of angulation deformity in the little metacarpal shaft varies from 25-40°.4
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: fracture line defining one or several fracture fragment fragments; however, the external cortical contours are not significantly disrupted
- A small percentage of little metacarpal shaft fractures treated conservatively with immobilization may eventually displace enough to warrant surgical intervention.17
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- Little metacarpal fractures can have fragment involvement with its MP or CMC joint.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
- Although intra-articular metacarpal base fractures generally occur infrequently, they are fairly common in the little metacarpal. These are high-energy injuries often concomitant with a CMC dislocation, and some have suggested that they may be underreported and underdiagnosed.2,11,18
- Differentiating between extra- and intra-articular fractures is crucial for planning an appropriate treatment protoco and may require CT scan evaluationl.2
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.7-9
Little metacarpal fractures: named fractures, fractures with eponyms and other special fractures
Little metacarpal neck fracture/Boxer’s fracture
- Fractures of the little metacarpal neck are the most common type of metacarpal fractures overall, and they are often referred to as boxer’s fractures. This term is considered to be a misnomer, since the injury is unlikely to occur in professional boxers, but it continues to be used in the literature nonetheless.1,16,19
- Boxer’s fractures account for approximately 25% of all metacarpal fractures and about 5% of all upper extremity fractures.6
- As the name suggests, the most common mechanism of injury is a punching force, in which axial pressure is applied to the little metacarpal with the fist in a clenched position. This force transfers energy to the metacarpal axially, which typically fractures the little metacarpal neck and results in apex dorsal angulation.
- Direct trauma to the dorsum of the hand may also cause this fracture, but it does not typically occur with a fall onto an outstretched hand, unlike many other hand and wrist fractures.16
- When displaced, boxer’s fractures can result in loss of strength, loss of extension range, rotational malalignment, and cosmetic disfigurement due to loss of the prominence of the little metacarpal head at the dorsal aspect of the hand.20
Imaging
- Anteroposterior, lateral, and oblique radiographic views are required.
- The lateral view should be used to measure the degree of angulation of the metacarpal shaft compared to the midpoint of the fracture fragment.16
- Ultrasound may also be used to make an initial diagnosis.
- CT scans are rarely used, but may help to detect occult fractures in patients with a high degree of clinical suspicion for fracture and negative plain radiographs.16
- The optimal management strategy for boxer’s fractures is still a matter of debate, and positive outcomes have been reached with both conservative and surgical interventions. Therefore, treatment protocols appear to be highly variable and based partially on personal preference.19,20
- The majority of boxer’s fractures are isolated injuries that are simple, closed, and stable, and conservative treatment is generally recommended for these injury patterns.19
Treatment
- When these fractures are closed and non-displaced without any angulation or malrotation, initial immobilization with an ulnar gutter splint is frequently utilized. Alternatively, a pre-made Galveston splint or a custom orthosis may be used.
- The hand should be positioned for splinting as follows: 20-25° wrist extension, 70-90° of flexion at the MP joint, and in extension or mild flexion at the distal interphalangeal (DIP) and proximal interphalangeal (PIP) joints.16
- When there is significant angulation in these fractures of greater than 30-40°, closed reduction and immobilization are typically required. Fractures with pseudo-clawing should also undergo closed reduction.
- Closed reduction is accomplished by using the “90-90 method, aka Jahss maneuver:” the MP, DIP, and PIP joints are all flexed to 90°, and the clinician applies volar pressure over the dorsal aspect of the fracture site while applying pressure axially to the flexed PIP joint.
- The injury should be subsequently immobilized with an ulnar gutter splint, and post-reduction films should be taken to assess for adequate reduction.16
- Unfortunately, some boxer’s fractures treated with closed reduction and immobilization tend to redisplace easily after reduction.19
- Alternative conservative treatments include use of a soft, compressive wrap with no reduction and immediate ROM and/or buddy taping.21
- Surgery is typically indicated for boxer’s fractures that are open, severely comminuted, associated with neurovascular injury, or when there is any malrotation or longitudinal shortening. It may also be appropriate if a fracture with significant angulation is unable to be adequately reduced and aligned non-surgically.16,19
- A number of surgical techniques have been utilized for treating boxer’s fractures, including intramedullary K-wires, transverse K-wires, tension bands, locked intramedullary nailing, external fixation, and locking plate fixation.22
- Some consider the standard surgical intervention for these fractures to be divergent intramedullary pinning, or bouquet pinning.
- This procedure has been proven effective but is challenging and tedious to perform, with increased operative time and risk of complications.
- These difficulties have prompted the development of alternative techniques, such as double L-shaped pinning, transverse pinning, retrograde pinning, and intramedullary nailing, but these techniques are also complex.
- Some authors therefore suggest a simple intramedullary pinning technique that uses a single thick K-wire.20
- After immobilization, passive and active ROM exercises should be performed to alleviate stiffness of the MP and PIP joints. If any loss of function persists after several weeks of these exercises, patients should be referred to occupational or physical therapy.16
Complications
- Skin necrosis
- Infection
- Complex regional pain syndrome
- Refracture
- Tendon injury
- Loss of reduction
- Extensor tendon rupture or adhesion
- Persistent pseudo-clawing
Outcomes
- One study concluded that current evidence suggests conservative treatment is the optimum treatment for boxer’s fractures based on reduced complication rates.
- Conversely, transverse pinning with K-wires was identified as the worst option in this series, with a high complication rate.
- Plate fixation and antegrade intramedullary nailing were associated with the best surgical outcomes, and authors recommended that these be considered as viable first-line surgical options, although it’s not clear which of them is superior.19
- Another study highlighted that prospective, randomized studies have shown that regardless of fracture angulation or treatment method, adequate short-term and long-term outcomes can be achieved with either closed reduction and splint immobilization or soft wrap without reduction.
- Results indicated that there was no benefit to reduction and splint immobilization for closed boxer’s fractures with initial angulation of less than 70°, and soft wrap without reduction was actually found to be generally favored in terms of MP ROM, strength, and swelling.
- The range of dorsal angulation that was accepted without reduction and placed in a soft wrap varied from 50-70°.
- Buddy taping was also identified as an effective conservative technique.
- A simple intramedullary pinning technique that uses a single thick K-wire was found to be a relatively simple, reproducible, and fast procedure that led to satisfactory clinical outcomes without inducing any rotational malalignment or any other complications.20
- One trial revealed that three-screw fixation of the distal fragment was superior to two-screw fixation, and this method may therefore reduce secondary displacement and improve overall clinical outcomes.22
- In a randomized-controlled trial that compared transverse pinning to intramedullary pinning, all patients achieved union and both techniques were deemed equally safe and effective, with the only difference being shorter operative time and fewer complications in patients treated with transverse pinning.23
Little CMC joint fracture-dislocation/Reverse Bennet’s fracture
- Fracture-dislocations of the little CMC joint resemble Bennett’s and Rolando’s fractures in their pattern and tendency to be unstable. For this reason, they are often referred to as “mirrored,” “reverse,” or “baby” Bennett’s fractures.24-26
- Despite its similarity to the Bennet’s fracture, little CMC fracture-dislocations have received far less attention in the medical literature.27
- Little CMC joint fracture-dislocations are commonly missed in clinical diagnosis, which means their true incidence is difficult to determine. Missing the diagnosis results in impaired function and weak grip, which is why it is crucial to recognize these injuries early.25
- The most common mechanism of injury is striking a hard object with a closed fist, while a fall on the wrist in forced flexion can also be responsible.25,26
- In most cases this force upon the metacarpal head causes a metacarpal neck fracture, but occasionally it results in an intra-articular base fracture.28
- Instability of these fractures is primarily due to the strong, unopposed proximal pull of the extensor carpi ulnaris (ECU), which causes ulnar and dorsal subluxation of the main fracture fragment.26,28
- Shortening of the little ray is also common in these injuries due to traction of the ECU tendon.24 Depending on the severity of the injury, other CMC joints can also be affected.25
- Displaced fracture-dislocations of the ring and little metacarpals are typically accompanied by a fracture of the dorsal hamate.
- Although relatively rare, isolated dislocation of the little CMC joint is also possible. These are usually high-energy injuries resulting from a directly blow transmitted to the dorsal and ulnar aspect of the little metacarpal. Dorsal isolated little CMC joint fracture-dislocations are more common than volar dislocations.29
Imaging
- Posteroanterior, oblique, and lateral views are usually sufficient for visualizing little CMC fracture-dislocations. CT scans are very useful during evaluation of the little CMC joint and reduce "missed" injuries.
Treatment
- Treatment for little CMC fracture-dislocations remains controversial with no clearly established guidelines on optimal treatment strategies, due primarily to a lack of clinical comparative evidence. Consequently, there are advocates behind both conservative and surgical approaches.26,27
- Conservative treatment typically consists of either cast immobilization or early-unrestricted mobilization.26
- The primary surgical treatment options include open reduction with internal fixation (ORIF) and closed reduction with percutaneous K-wire fixation.18,25
- Some experts claim that these injuries should be treated immediately by reduction and fixation because of their tendency to sublux or dislocate, resulting in post-traumatic arthritis in neglected injuries.24
- Closed reduction with percutaneous K-wire fixation appears to be more commonly recommended, but the procedure is associated with complications.18
- For patients with persistent pain, other surgical options include arthrodesis of the little metacarpal to either the hamate or ring metacarpal, partial resection arthroplasty, CMC joint suspension arthroplasty, and silastic or tendon interposition arthroplasty.24
- Isolated little CMC joint dislocations can be managed conservatively if diagnosed early, but if the initial reduction is unstable or there is delay in diagnosis or presentation, K-wire fixation after closed or open reduction is typically needed.29
Complications
- Impaired grip strength
- Stiffness
- Malunion
- Little CMC joint post-traumatic arthritis
Outcomes
- One systematic review reported that although the current literature indicated that most little CMC fracture-dislocations were treated surgically, these decisions were not evidence-based. Instead, the limited literature reviewed suggested that better functional outcomes could be achieved by early mobilization and conservative management, despite poorer anatomical restoration.25
- One study found that closed reduction with cast immobilization was an adequate and reliable treatment method little CMC fracture-dislocations, with all fractures healing quickly and all active duty military patients being able to return to full duty status after an average of 6 weeks.28
- Another study analyzed 64 little CMC fracture-dislocations treated with either closed reduction and casting or ORIF.
- Alignment was improved in 63% of fractures treated with ORIF, compared to only 20% of those treated conservatively. The authors therefore recommend ORIF for displaced fractures to restore the articular surface.30
- One study found that little CMC fracture-dislocations treated with plaster immobilization were unstable, while those treated with percutaneous K-wires were less unstable, and those treated with ORIF experienced adhesions and stiffness.
- An acceptable alternative that allows immediate mobilization is a percutaneous locked K-wire technique, which combines non-traumatic closed reduction, percutaneous pin fixation, and solid fixation using an external connector.18
- One trial found that suspension arthroplasty using a partial slip of the ECU tendon led to positive outcomes and offered advantages over other techniques for degenerative arthrosis of the little CMC joint.24
- The proponents of surgical management have shown that grip weakness, longer periods of disability, and poorer outcome in patients with inadequate reduction of little CMC fracture-dislocations, while those who support conservative treatment have reported the contrary. Regardless of their choice of treatment option, a surgeon’s personal preference will be supported by evidence-based literature.26
Related Anatomy
- The little metacarpal consists of a distal head that articulates at the MP joint with the proximal phalanx, a supportive neck, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the little CMC joint with the ring metacarpal and the hamate. The proximal surface of its base is a facet that is concave from side to side and convex from its volar to dorsal aspect, for articulation with the hamate. Its lateral aspect features an elongated strip-like facet for articulation with the ring metacarpal.24,27
- Ligamentous attachments of the little metacarpal include the pisometacarpal ligament, which is a distal extension of the flexor carpi ulnaris (FCU) that attaches to the base of the little metacarpal, the deep transverse metacarpal ligament, natatory ligament, an interosseous ligament and the dorsal carpometacarpal ligament that attaches to the hamate.27
- The tendons associated with the little metacarpal include the ECU tendon, which passes through the ECU groove of the ulna and inserts at the dorsalulnar aspect of the base of the little metacarpal, and the FCU tendon. The ECU functions not only as the ulnar wrist extensor and ulnar deviator, but also as the dynamic stabilizer of the distal radio-ulnar joint.27
- The shallow saddle-shaped bony configuration of the little CMC joint provides intrinsic stability but allows an average of 30° flexion-extension.24
Incidence and Related injuries/conditions
- Metacarpal and phalangeal fractures account for nearly half of all hand injuries that present to the emergency room.31
- Metacarpal fractures are less common than phalangeal fractures, but comprise between 18-44% of all hand fractures.32,33
- It is estimated that over 250,000 metacarpal fractures occur in the U.S. each year.32
- One study reported an overall incidence rate of 13.7 metacarpal fractures per 100,000 person-years, with these injuries comprising 33% of all hand fractures in the U.S.3
- About 88% of all metacarpal fractures occur in non-thumb metacarpals, with the little metacarpal being most commonly involved.32
- In one study that included 400 participants, fractures of the little metacarpal represented 75.5% of all metacarpal fractures, which was followed by the ring metacarpal (16.3%), long metacarpal (4.1%), and index metacarpal (4.1%).34
- In another study on 785 participants, the little finger sustained 302 fractures, or 38% of all fractures distal to the carpal bones, which was primarily due to the high prevalence of little metacarpal fractures (11% of all hand fractures).5
- More specifically, little metacarpal neck fractures are the most common of all metacarpal fractures, representing approximately 25% of all metacarpal fractures and 5% of all upper extremity fractures.6
- One trial investigated the distribution of 49 fractures throughout the little metacarpal and found that 34 (69.4%) occurred in the neck, 11 (22.4%) in the shaft, 4 (8.2%) in the base, and 0 (0%) in the head.35
- Men between the ages of 10-29 have been identified as the population with the highest incidence of metacarpal fractures, with a peak incidence between ages 10-19.3
- Punching a wall or door is by far the most common mechanism of injury for metacarpal fractures, especially those of the little metacarpal, while sporting activities—particularly football and basketball—account for the next largest portion.12
- Another study found that bicycle accidents also accounted for a large proportion of metacarpal fractures across all demographics, while accidental falls were the mechanism of injury over a bimodal distribution of age groups younger than 9 and older than 50 years old.3
- An additional trial found that aggression was involved in approximately half of all little metacarpal fractures and that the dominant hand was affected more frequently than the non-dominant hand.36