Fracture Nomenclature for Finger Distal Phalanx Fractures
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Finger Distal Phalanx, the historical and specifically named fractures include:
Mallet finger fracture
FDP tendon avulsion fracture
DIP joint volar plate avulsion fracture
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Fractures of the distal phalanx are the most common fractures that occur in the hand.1-3
Definitions
- A distal phalanx fracture is a disruption of the mechanical integrity of the distal phalanx.
- A distal phalanx fracture produces a discontinuity in the distal phalanx contours that can be complete or incomplete.
- A distal phalanx fracture is caused by a direct force that exceeds the breaking point of the bone.
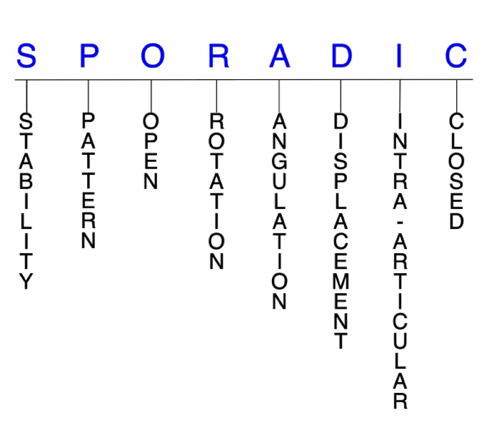
- The mechanism of injuries that lead to distal phalanx fractures like falls, sports and motor vehicle accidents are common. But the occurrence of a fracture in a particular human is sporadic. Thus the acronym below is appropriate for systematically describing fractures.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.4-6
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragments’ alignment is maintained by with simple splinting. Most published definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable distal phalanx fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
P - Pattern
- Distal phalanx tuft: oblique, transverse, or comminuted
- Distal phalanx shaft: transverse, oblique, or comminuted with or without shortening
- Distal phalanx base: can involve the distal interphalangeal (DIP) joint; these intra-articular fractures usually involve the dorsal or volar lip of the distal phalanx base
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the distal phalanx require antibiotics with surgical irrigation and wound debridement.4,7,8
R - Rotation
- Distal phalanx fracture deformity can be caused by proximal rotation of the fracture fragment in relation to the distal fracture fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity; this is not a common type of fracture deformity in the distal phalanx.
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- Example: distal phalanx shaft fracture with an angulation of 45° could have the apex of the angulation dorsally or volarly
D - Displacement (Contour)
- Displaced: disrupted cortical contours (eg, distal phalanx shaft fractures can be displaced or translated partially or completely)
- Nondisplaced: fracture line(s) defining one or several fracture fragment fragments; however, the external cortical contours are not significantly disrupted
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- Distal phalanx fractures can have fragment involvement with the DIP joint.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.4-6
Distal phalanx fractures: named fractures, fractures with eponyms and other special fractures
Mallet finger fracture
- Fracture-dislocation of the DIP joint caused by avulsion of the dorsal lip of the distal phalanx. The mallet finger fracture is usually unstable when >50% of joint is involved.4,8,9
- Patients are typically younger with a history of a sports-related accident.10
- Usually occurs when the tip of the finger is struck with a severe axial load that drives the tip volarly faster than the extensor can relax (eg, when a baseball strikes the fingertip).
- The ring finger is the most commonly injured finger.10
- Examination typically shows a swollen and ecchymotic DIP joint with marked dorsal tenderness4,8,10 and positioned in flexion.
- Active ROM exam demonstrates an active extension lag. The collateral ligaments and volar plate are stable.
- Flexor digitorum profundus (FDP) tendon function is intact with normal sensation and normal capillary refill.
Imaging
- Plain AP and lateral X-rays show the dorsal lip fracture.
- The amount of articular surface involvement and degree of volar subluxation of the distal phalanx is best calculated on the lateral X-ray.
Treatment
- Splinting the DIP joint in extension is the mainstay of treatment for the majority of mallet finger fractures.4,8,10
- Splinting can be done with an aluminum-padded splint, plaster cast, prefabricated commercial splint, or custom splint.
- Most hand surgeons agree that there are 3 mallet finger fracture patterns that always warrant surgical intervention:
- Large dorsal lip fracture fragment representing 25-50% of joint surface; the exact percentage is not well defined
- Dorsal lip fracture associated with volar subluxation of the large distal phalanx fracture fragment
- Dorsal lip fracture fragment that has been pulled proximally over the neck of the middle phalanx
- When one of more of these surgical indications is present, reconstructive surgical options include extension block splinting, ORIF with screw, pin, plate, pullout suture or wire.4,8,10
Complications
- Posttraumatic osteoarthritis
- Swan neck deformities
- Dorsal prominence at the DIP joint
Outcomes
- Most patients do well. If the dorsal lip represents ≤1/3, then splinting results are essentially the same as surgical treatment results.
- Results are better if treated within 2 weeks.11
- No surgical procedure appears to be better than any other.8
FDP tendon avulsion fracture
- Avulsion of the volar lip of the distal phalanx; also called the "jersey finger" injury.
Imaging
Treatment
- Asymptomatic late cases can be left untreated.12
- Timing is critical for successful repair. Some types require immediate surgery, owing to disruption of the blood supply to the distal tendon;13 others can be delayed.14
- Options for late interventions: two-stage tendon graft or fusion of DIP joint if unstable.12
Complications
- In conservatively managed cases, the necrotic tendon may lead to tenderness in the palm and require excision.
- Extension deficit due to flexor tendon advancement during repair
- DIP joint stiffness
- Operative repair that damages the volar plate may lead to flexion contracture.12
Outcomes
- In one study, 100% (12/12) patients had satisfactory results after tendon reinsertion; there was a 10–15° extension deficit but good flexion and, in patients treated early, grip strength approached normal values.12
- Although several repair methods have been developed, none has yet been shown to result in a superior clinical outcome.15,16
DIP joint volar plate avulsion fracture
- A DIP joint volar plate avulsion fracture can occur at the proximal portion of the volar distal phalanx lip without disrupting the insertion of the FDP. This uncommon distal phalanx fracture is associated with dorsal subluxation of the larger distal phalanx fracture fragment.6&20
- This fracture occurs when an axial load is applied to the fingertip while the DIP joint is in slight flexion. This axial loading causes the volar lip of the distal phalanx to be avulsed by the volar plate or a significant comminuted fracture of the distal phalanx lip occurs as the distal phalanx is impacted on the head of the middle phalanx.
Imaging
- Plain x-ray imaging will define these fractures very well. Careful attention should be given to the true lateral view.
Treatment
- Volar plate avulsion fractures of the distal phalanx that are seen acutely can be reduced and DIP joint stabilized by first obtaining a closed reduction and then securing the reduction with percutaneous pinning of the DIP joint. Splinting alone of the reduced fracture dislocation is unlikely to keep the joint anatomically aligned.
- In chronic cases open reduction and internal fixation; open reduction and pinning; dynamic traction; volar plate advancement arthroplasty; and/or DIP joint arthrodesis have all been successfully used to treat this fracture problem successfully.17
Complications
- Distal interphalangeal joint pain
- Distal interphalangeal joint stiffness and flexion contracture
- Distal interphalangeal joint osteoarthritis
- Infection can complicate any open treatment options.
Outcome
- When the DIP joint congruity and stability are obtained either acutely or chronic situation by reconstructive surgery then the clinical outcome is usually good to excellent.
Related Anatomy18
- The distal phalanx consists of a distal bony tuft, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the DIP joint with the middle phalanx. The base of the distal phalanx has a dorsal and volar lip.
- Ligaments that attached to the distal phalanx include the volar plate of the DIP joint, the radial collateral ligament of the DIP joint and the ulnar collateral ligament of the DIP joint.
- Tendon insertions include the insertion of the terminal extensor tendon into the dorsal lip of the distal phalanx and the insertion of the flexor digitorum profundus into the volar proximal third of the distal phalanx.
- The distal phalanx and fingertip are further stabilized by fibrous septae in the pulp of the finger and ulnar and radial lateral interosseous ligaments between the base and tuft of the distal phalanx.
Incidence and Related injuries/conditions
- The most commonly fractured bone in the human hand is the distal phalanx.1,3
- Distal phalanx fractures are the most commonly occurring hand fracture.
- Distal phalanx fractures occur most commonly secondary to sports in younger patients, secondary to labor in middle-aged patients and secondary to falls and motor vehicle accidents in older individuals.8
- Subungual hematomas are a common related injury.