Fracture Nomenclature for Trapezoid Fractures
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Trapezoid Fracture, the historical and specifically named fractures include:
Trapezoid dislocations and fracture-dislocations
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Fractures of the carpal bones account for ~6% of fractures overall and up to 18% of all hand fractures. The vast majority (58-89%) occurs in the scaphoid, while fractures of the other 7 carpals are uncommon and only comprise ~1.1% of all fractures. The trapezoid is the least commonly fractured of the carpal bones, with a reported incidence of 0.4-1% of all carpal fractures. This is primarily due to the stability of the trapezoid. Trapezoid fractures rarely occur in isolation and are more frequently associated with other injuries, such as fractures of adjacent carpal bones and disruptions at the carpometacarpal (CMC) and intercarpal joints. Most experts agree that conservative treatment is indicated for nondisplaced and minimally displaced fractures, while surgery is often required for displaced cases, those with articular incongruity, and after nonuion.1-5
Definitions
- A trapezoid fracture is a disruption of the mechanical integrity of the trapezoid.
- A trapezoid fracture produces a discontinuity in the trapezoid contours that can be complete or incomplete.
- A trapezoid fracture is caused by a direct force that exceeds the breaking point of the bone.
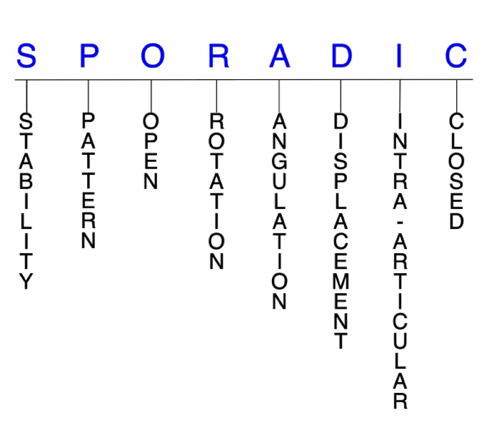
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.6-8
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragment’s alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable trapezoid fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
P - Pattern
- Trapezoid dorsal rim
- Trapezoid body
- Can be sagittal, coronal, and/or comminuted.3,4
- When an isolated trapezoid fracture is displaced enough to be see on radiographs, it usually has a characteristic coronal orientation.4
- The most common mechanism of injury is an axial load through a flexed index metacarpal, which drives the metacarpal proximally and displaces the trapezoid dorsally.
- Other less common mechanisms include direct trauma and forced flexion-extension through the index MP joint.4,5
- Due to the rigid stability of the trapezoid within the carpus, high-energy trauma is needed to fracture the bone. This is why associated fractures of surrounding bones are so common.4
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the trapezoid require antibiotics with surgical irrigation and wound debridement.6,9,10
- Open fractures of the trapezoid may require surgical exploration to determine if articular surfaces are involved. After irrigation and debridement, these wounds are generally left open and further treatment is typically delayed until the wound shows no sign of infection.11,12
- Since high-energy trauma is often needed to cause a trapezoid dislocation, some of these injuries are open.
R - Rotation
- Trapezoid fracture deformity can be caused by rotation of the distal fragment on the proximal fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: fracture line defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
- Displaced trapezoid fractures may occur concomitantly with an associated dislocation of the trapezoid or index metacarpal.3
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- Trapezoid fractures can have fragment involvement at the index CMC joint or at any of its intercarpal joint articulations.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.6-8
Trapezoid fractures: named fractures, fractures with eponyms and other special fractures
Trapezoid dislocations and fracture-dislocations
- Dislocations of the trapezoid are extremely rare injuries that usually occur in conjunction with other hand and wrist injuries. Isolated trapezoid dislocations are even less common.3,13
- The most common associated injuries are other carpal fractures, trapezium dislocations, and multiple CMC dislocations and fracture-dislocations.13
- Trapezoid dislocations typically result from high-energy trauma, and possible mechanisms of injury include industrial trauma, motorcycle accidents, and falls from a height. They have also been described as steering wheel injuries, which are caused by powerful axial loading force on the dorsal hand when grasping something strongly.
- Because many trapezoid dislocations result from serious accidents, they may not be prioritized over other life-threatening injuries. Associated soft-tissue injuries are also common.13,14
- Dorsal dislocations are far more common than volar dislocations because the volar ligamentous attachments of the trapezoid are stronger than the dorsal ligaments.13
- Trapezoid fracture-dislocations, in particular, tend to be dorsal and may involve an avulsion of the volar ligaments.3
Imaging
- Trapezoid dislocations can be missed or ignored because of other life-threatening complications, local swelling, and/or confusing X-rays. A high index of clinical suspicion should be maintained after high-energy injuries to prevent a delayed diagnosis.13,14
- A straight posteroanterior (PA) radiographic view may be helpful; however, X-rays are often not reliably accurate for diagnosing trapezoid dislocations because of the high prevalence of concomitant injuries.13
- CT scan
- Utilized by some surgeons for any high-energy injuries suspected of trapezoid dislocation, because it can more accurately identify injuries when radiographs are inconclusive.14
Treatment
- There is no consensus regarding the optimal treatment of trapezoid fractures and fracture-dislocations, with different authors reporting a variety of approaches.13
- Some surgeons insist that anatomical reduction is essential for obtaining a good result, while others have reported that trapezoid resection and limited intercarpal fusion without anatomical reduction is also a viable route.13
- Closed reduction and percutaneous pinning (CRPP)
- Can be attempted for some closed trapezoid fracture-dislocations, but the success rate id low.15,16
- Open reduction and internal fixation (ORIF)
- Often necessary if CRPP fails.16
- Limited intercarpal fusion with trapezoid resection
- May be a useful option for chronic trapezoid dislocations.13
- Whatever surgical intervention is utilized, soft tissue preservation should be a priority for all surgeons.17
Complications
- Infection
- Avascular necrosis
Outcomes
- Although the management of isolated trapezoid dislocations varies considerably, most patients experience reasonably good outcomes regardless of the treatment used.15
- Closed reduction has not been successful for treating volar trapezoid dislocations.17
Related Anatomy
- The trapezoid is an irregular, wedge-shaped bone that consists of a dorsal rim and a body. It is the smallest of the carpals in the distal row and is considered the keystone of the carpal arch, with its dorsal surface being widest and approximately twice the size of its volar surface. The trapezoid articulates with the scaphoid proximally, the capitate ulnarly, the trapezium radially, and the index metacarpal distally.3,18
- Ligamentous attachments include the trapeziotrapezoid, trapeziocapitate, dorsal and volar CMC, dorsal intercarpal, and triscaphe ligaments. These stout ligaments and the position of the trapezoid keep it protected from most injuries and transfers axial-loaded forces from the index metacarpal base into the scaphoid.3,4,18
- Tendons associated with the trapezoid include the deep head of flexor pollicis brevis, which originates from its volar surface, and the oblique head of the adductor pollicis, which originates from its distal ulnar volar surface.3
Incidence and Related injuries/conditions
- Fractures of the carpal bones have been found to account for 8-18% of all hand fractures19,20 and ~6% of fractures overall.21
- Fractures of the proximal carpals are more common than the distal carpals.
- Most commonly fractured carpal bone is the scaphoid, representing 58-89% of all carpal fractures.19,20,22,23
- Other carpal fractures are rare and only account for ~1.1% of all fractures. The triquetrum ranks highest of these bones, while fractures of the remaining carpals are even less common and incidence estimates vary.24-26
- Trapezoid fractures are the least commonly fractured carpal, having a reported incidence of 0.4-1% of all carpal fractures.26-28
- Most trapezoid fractures are associated with other carpal bone injuries.
- In a large case series at a level 1 trauma center over 3 years in, 95% of trapezoid fractures involved concomitant wrist injuries.4