Fracture Nomenclature for Trapezium Fracture
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Trapezium Fracture, the historical and specifically named fractures include:
Trapezium dislocations and fracture-dislocations
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Fractures of the carpal bones account for ~6% of fractures overall and up to 18% of all hand fractures. The vast majority (58-89%) occurs in the scaphoid, while fractures of the other 7 carpals are uncommon and only comprise ~1.1% of all fractures. Trapezium fractures make up 1-5% of all carpal fractures, but these injuries are important to detect and treat appropriately due to the crucial role of the trapezium in thumb carpometacarpal (CMC) movements. The mechanism of injury is believed to be either indirect trauma—such as a fall on an outstretched hand (FOOSH)—that compresses the trapezium between the thumb metacarpal and radial styloid, or a direct trauma in which the thumb is driven into the trapezium. Although isolated trapezium fractures do occur, they are more commonly seen with other injuries, such as Rolando’s and Bennett’s fractures, or fractures of the scaphoid, capitate, or metacarpals. Conservative treatment is often indicated for most nondisplaced fractures, while surgery is required in displaced cases and those that cannot be reduced nonsurgically.1-5
Definitions
- A trapezium fracture is a disruption of the mechanical integrity of the trapezium.
- A trapezium fracture produces a discontinuity in the trapezium contours that can be complete or incomplete.
- A trapezium fracture is caused by a direct force that exceeds the breaking point of the bone.
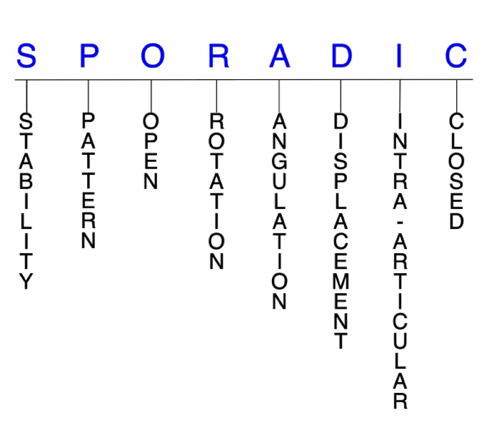
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability are not well defined in the hand surgery literature.6-8
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragment’s alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable trapezium fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
- Longitudinal injuries at the thumb CMC joint are typically unstable and may be associated with subluxation of the thumb metacarpal.4
P - Pattern
- Trapezium ridge (radial tubercle): typically isolated and caused by axial loading or avulsion by the transverse carpal ligament during a FOOSH injury2
- Palmer classified trapezium ridge fractures into 2 types:
- Type 1: involve the base of the ridge; typically heal with immobilization alone
- Type 2: involve the tip of the ridge and are usually avulsion injuries that have a higher incidence for symptomatic nonunion10
- Trapezium body: Usually result from an axial compression force from the thumb metacarpal and are accompanied by a Bennett’s fracture.3, 4, 12
- horizontal, vertical, sagittal, coronal, and/or comminuted1, 3, 11
- Vertical, intra-articular fractures are the most common pattern.
- According to one study, about 20% of trapezium fractures are vertical sagittal split fractures.4
- Horizontal fractures typically occur due to a horizontal shear load against the trapezium.3
- Trapezium fractures can also be diagnosed using the Walker1, 13classification system:
- Type I: horizontal body fracture
- Type II: ridge fracture
- Type IIa: involves the CMC joint
- Type IIb: involves the scaphotrapezial joint
- Type III: ulnar tubercle fracture
- Type IV: vertical body fracture
- Type V: comminuted body fracture
- There is no consensus on the mechanism of injury of trapezium fractures, but it appears that most are caused by one of the two following forces:
- An indirect trauma by a FOOSH, where the hand goes into hyperextension and radial deviation and the trapezium gets compressed between the base of the thumb metacarpal and radial styloid.
- A direct trauma to the dorsoradial aspect of the hand in which the thumb is driven into the trapezium.4, 5
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the trapezium require antibiotics with surgical irrigation and wound debridement.6, 14, 15
- Many trapezium dislocations are open because they often result from a grinding or crushing force and there is a high likelihood of extensive associated soft tissue damage.16
R - Rotation
- Trapezium fracture deformity can be caused by rotation of the distal fragment on the proximal fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: fracture line defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
- In vertical trapezium fractures, displacement occurs frequently due to forces exerted by the abductor pollicis longus muscle.17
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- Trapezium fractures can have fragment involvement with any of its CMC or intercarpal joint articulations.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to post-traumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of post-traumatic osteoarthritis increases significantly.
- Vertical intra-articular trapezium fractures have been reported as the most common fracture pattern and usually result from an axial compression force from the thumb metacarpal.3
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.6-8
Trapezium fractures: named fractures, fractures with eponyms and other special fractures
Trapezium dislocations and fracture-dislocations
- Trapezium dislocations are relatively rare, even among carpal dislocations. Most of these injuries occur concomitantly with a fracture of another surrounding bone—usually the scaphoid, trapezoid, capitate, thumb or index metacarpals, or distal radius—while isolated dislocations are possible but even less common.3, 16
- The most common mechanisms of injury are a direct blow and a crush injury, and a high-energy force is typically needed to cause a trapezium dislocation. The trapezium’s strong dorsal ligamentous attachments ensure that a traumatic force will usually result in a thumb metacarpal fracture rather than a trapezium dislocation.16, 18
- Trapezium dislocations tend to occur in either a volar or a radiodorsal direction, with the former being far more common because of the relative strength of the radial and palmar scaphotrapezial ligament complex.16, 19
Imaging
- Oblique, pronated oblique, straight posteroanterior (PA), and Robert’s radiographic views are all particularly useful for identifying trapezium dislocations and fracture-dislocations.18, 19
- Recognizing these injuries can be difficult because Gilula’s three arcs do not account for the position of the trapezium as originally described. Careful radiographic evaluation is therefore necessary.18
- A CT scan may also be needed in certain suspected cases.18, 19
Treatment
- There is no consensus regarding the optimal management of these injuries on account of their rarity, and current treatment recommendations are therefore unclear.9
- Options include closed reduction with or without K-wire fixation and immobilization, open reduction with K-wire fixation, and salvage procedures.19
- Conservative treatment using cast or splint immobilization may be possible if the joint is stable, but surgery is typically needed otherwise.9
- Open reduction with K-wire fixation
- Should be employed if the fracture is unstable or open, or if there is a failure to achieve adequate reduction. Some authors even advocate for it regardless of whether the injury is open or closed.16
- Trapezium excision may be required in cases of isolated dislocation when reduction is not possible through other means, but this option is generally considered a salvage technique only and is rarely used.16
- Arthrodesis is another salvage procedure that may be used when open reduction cannot be obtained or maintained.19
Complications
- Decreased ROM
- Decreased grip and pinch strength
- Posttraumatic osteoarthritis
- Osteonecrosis
- Carpal instabilities
Outcomes
- Outcomes after isolated trapezium dislocations are reduced are generally satisfactory, although loss of ROM and decreased grip and pinch strength may occur.19
- In the majority of reported cases, percutaneous fixation using K-wires has been identified with acceptable results.16
- Three reports have demonstrated excellent patient outcomes with closed reduction and percutaneous pinning (CRPP), while 7 cases have demonstrated excellent outcomes with open reduction and percutaneous fixation.18
Related Anatomy
- The trapezium is an irregular-shaped bone located in the most radial position of the distal carpal row that consists of a ridge—or radial tubercle—a body, an ulnar tubercle, and a deep groove on its anterior surface. It articulates distally with the thumb metacarpal at the thumb CMC joint, medially with the index metacarpal at the index CMC joint and with the trapezoid at the triscaphe joint, and proximally with the scaphoid at the scaphotrapezial joint. The trapezium also forms the radial border of the carpal tunnel.
- Ligamentous attachments of the trapezium include
- Two layers of the flexor retinaculum, which attach on either side of its deep groove.
- The anterior oblique ligament, which anchors the volar lip of thumb metacarpal to tubercle of the trapezium.
- The radial collateral ligament and capsule of the thumb CMC joint, both of which attach to the lateral surface of the trapezium.
- Tendons associated with the trapezium include the superficial head of flexor pollicis brevis, opponens pollicis, and abductor pollicis brevis tendons, all of which arise from the trapezium ridge.
Incidence and Related injuries/conditions
- Fractures of the carpal bones have been found to account for 8-18% of all hand fractures,20, 21and ~6% of fractures overall.22
- Fractures of the proximal carpals are more common than the distal carpals, and the most commonly fractured carpal bone is the scaphoid, which represents 58-89% of all carpal fractures.20, 21, 23, 24
- Fractures of the other 7 carpals are very rare and only account for ~1.1% of all fractures. The triquetrum ranks highest of these bones, while fractures of the remaining carpals are even less common and vary in incidence.25-27
- Trapezium fractures account for 1-5% of all carpal fractures.28, 29
- According to one source, the trapezium is the third most commonly fractured carpal bone, but this statistic does not appear to be universally accepted.28