Fracture Nomenclature for Scaphoid Fractures and Fracture Dislocations
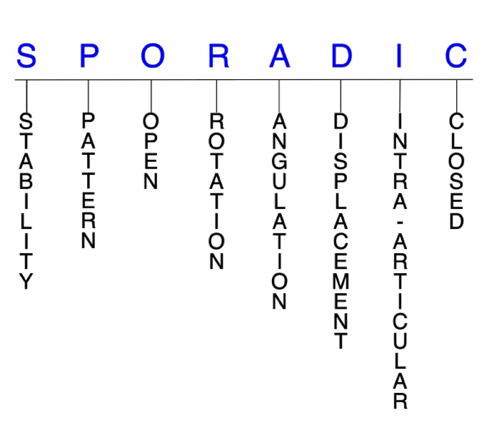
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Scaphoid Fractures and Fracture Dislocations, the historical and specifically named fractures include:
Scaphocapitate fracture syndrome
Scaphoid dislocation and fracture-dislocation
Scaphoid avulsion fracture
Trans-scaphoid perilunate dislocation and fracture-dislocation
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Fractures of the carpal bones account for ~6% of fractures overall and up to 18% of all hand fractures. The vast majority (58-89%) occur in the scaphoid, while fracture of the other 7 carpals is very uncommon and only comprise ~1.1% of all fractures. Scaphoid fractures represent 2-7% of all orthopedic fractures and are second only to the distal radius in terms of frequent wrist injuries. They are most often seen in young men and the typical injury mechanism is forced wrist dorsiflexion, often from a fall on an outstretched hand (FOOSH), although direct blows and axial loading may also be responsible. Treatment for scaphoid fractures is controversial and preferences vary between treatment centers, but it is generally agreed that conservative treatment with cast immobilization is appropriate for nondisplaced and minimally displaced fractures, especially those in the distal third. Surgery is usually required for most proximal pole fractures, nondisplaced or unstable fractures, and cases that fail conservative interventions, as well as for nonunion after treatment, which is common. Prompt diagnosis and suspicion of scaphoid fractures can help increase the chances of a successful outcome and reduce the risk of complications.1-7
Definitions
- A scaphoid fracture is a disruption of the mechanical integrity of the scaphoid.
- A scaphoid fracture produces a discontinuity in the scaphoid contours that can be complete or incomplete.
- A scaphoid fracture is caused by a direct force that exceeds the breaking point of the bone.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability are not well defined in the hand surgery literature.8-10
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragment’s alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable scaphoid fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
- The most commonly used classification system for scaphoid fractures is the Herbert classification, which is helpful because it specifically defines stable and unstable fractures.
- Type A: stable
- Type A1: fracture of tubercle
- Type A2: incomplete fracture through waist
- Type B: unstable
- Type B1: distal oblique fracture
- Type B2: complete fracture of waist
- Type B3: proximal pole fracture
- Type B4: trans-scaphoid perilunate fracture-dislocation
- Type B5: comminuted fracture
- Type C: delayed union
- Type D: established non-union
- Type D1: fibrous union
- Type D2: pseudoarthrosis
- Type D3: sclerotic pseudoarthrosis
- Type D4: avascular necrosis11
- In the Russe classification system, scaphoid fractures are more simply categorized as horizontal oblique, vertical oblique, or transverse. Under to this system, vertical oblique fractures only account for 5% of scaphoid fractures but result in the most shear forces across the fracture site, making it the least stable of these fracture types.3,12
P - Pattern
- Scaphoid tubercle: only account for ~8% of scaphoid fractures.13
- Caused by direct impact with the hand in dorsiflexion, ulnar deviation, and pronation, leading to a fragment avulsion by the radial collateral ligament, capsular attachments, or transverse carpal ligament14
- Scaphoid distal pole: usually oblique
- Account for ~10% of scaphoid fractures13
- Scaphoid waist: transverse, vertical oblique, horizontal oblique, coronal, and/or comminuted; can be complete or incomplete
- The most common fracture site, accounting for ~65% of all scaphoid fractures.13
- Compressive forces are seen at the fracture site in horizontal oblique fractures, while transverse fractures have a combination of shear and compressive forces.3
- Coronal fractures are rare and often missed and may be either complete and involve the entire waist, or partial and involve either the proximal or distal pole.15
- Scaphoid proximal pole: unstable fractures that are difficult to treat2
- May be easily missed on plain radiographs.3
- Account for ~15% of scaphoid fractures.13
- The usual mechanism of injury in scaphoid fractures is a forced dorsiflexion wrist injury—most commonly a FOOSH with a pronated and ulnarly deviated hand, and the wrist typically in wrist hyperextension past 95°—which causes longitudinal loading of the scaphoid and a subsequent fracture as the volar cortex fails in tension. The force then extends to the dorsal cortex, which fails in compression. Other possible injury mechanisms include a direct blow or axial loading with the wrist in neutral flexion-extension.2-4
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the scaphoid require antibiotics with surgical irrigation and wound debridement.8,16,17
- Open fractures of the scaphoid may require surgical exploration to determine if articular surfaces are involved. After irrigation and debridement, these wounds are generally left open and further treatment is typically delayed until the wound shows no sign of infection.18,19
R - Rotation
- Scaphoid fracture deformity can be caused by rotation of the distal fragment on the proximal fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
- Scaphocapitate fracture syndrome consists of concomitant fractures of the scaphoid and capitate with a rotation of 90-180° of the proximal fragment of the capitate.20
- Opposing rotational moments on the proximal and distal poles cause dorsal angulation in scaphoid fractures.4
- The violent dorsiflexion force involved in most scaphoid often causes the scaphoid to rotate out of its correct anatomical position while maintaining the integrity of the ligaments supporting the lunate, triquetrum, and hamate.21
- With a fracture to its waist, the distal scaphoid rotates around the radioscaphocapitate ligament into an abnormal flexion, ulnar deviation, and pronation posture, while the lunate and attached proximal part of the scaphoid rotate into an abnormal extension, supination, and radial deviation.22
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- Failure to recognize a scaphoid fracture may result in humpback deformity of the scaphoid and dorsal angulation of the lunate—or dorsal intercalated segmental instability (DISI) deformity—which is caused by opposing rotational moments on the proximal and distal scaphoid poles.3,4
- Some authors have defined displacement in scaphoid fractures as a gap of 1 mm on plain radiographs, scapholunate angle of >60°, or a radiolunate angle of >15°.3
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: fracture line defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
- The majority of scaphoid fractures are stable and nondisplaced.
- Fracture displacement of >1 mm is associated with instability and is an indication for surgical intervention—such as open reduction and internal fixation (ORIF)—since these fractures heal more slowly, require longer immobilization, and are associated with a higher risk of non-union and post-traumatic osteoarthritis.4,7
- Vertical oblique scaphoid fractures are more likely to be displaced by shear forces, while horizontal oblique and transverse fractures have greater compressive forces and are less likely to be displaced.23,24
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- Scaphoid fractures can have fragment involvement with the radius or any of its intercarpal joint articulations.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to post-traumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised, and the risk of post-traumatic osteoarthritis increases significantly.
- Scaphoid fractures have a tendency for nonunion due to the nature of intra-articular fractures and the vulnerable vascularity of the proximal fragments.7
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.8-10
- Whether a trans-scaphoid perilunate fracture-dislocation is open or closed is one of the major factors that will help determine its clinical outcome.25
Scaphoid fractures: named fractures, fractures with eponyms and other special fractures
Scaphocapitate fracture syndrome
- Rare but complex injury that is typically considered a manifestation of the perilunate injury pattern.1,26
- Some believe this injury represents the final stage of a greater arc injury, but the different degrees and directions of displacement of the capitate head imply that it does not have a unique mechanism.20,26,27
- Most commonly occurs in young men between ages 20-30.28
- The most recognized mechanism of injury is a volar-applied force to a hyperextended wrist, such as from a fall from a height or vehicular accident.28
- This wrist hyperextension results in a scaphoid fracture and, with further extension, the capitate impacts on the dorsal lip of the radius. This produces a transverse capitate body fracture, in which its proximal fragment rotates 90-180° in the sagittal plane as the hand returns to a neutral position.1
- Can be either isolated or associated with a perilunate dislocation, but a substantial force is usually required to cause a dislocation.28
- In one study, scaphocapitate fractures were classified into the following 6 types based on fragment geometry and displacement:
- Type I: transverse fracture of the scaphoid and capitate without dislocation
- Type II: inverted proximal fragment of capitate that remains in articulation with the lunate
- Type III: dorsal perilunate dislocation
- Type IV: volar perilunate dislocation of the carpus and proximal fragment of the capitate
- Type V: isolated volar dislocation of the proximal fragment of the capitate
- Type VI: isolated dorsal dislocation of the proximal fragment of the capitate26
Imaging
- Plain radiographs may not show the extent of the median nerve lesion. This, combined with the rarity and complexity of these injuries, causes many diagnoses to be initially missed or incorrectly labelled as simple scaphoid fractures.20,26
- If plain radiography does not lead to a satisfactory diagnosis, a CT scan may be needed, especially if a complex carpal lesion is suspected.20,26
Treatment
- Some controversy exists about the optimal management strategy for these injuries, but it appears that conservative treatment—consisting of closed reduction and cast immobilization—may be appropriate for some nondisplaced scaphoid and capitate fractures.26
- For displaced or comminuted fractures, ORIF is generally considered the treatment-of-choice to reduce complications. The aim of treatment is reduction and fixation of both fractures to obtain bony union.
- A dorsal approach is most commonly used, while a volar approach is usually reserved for when decompression of the median nerve is necessary.22
- K-wires or compression screws are typically recommended to achieve fixation and reduce the risk for nonunion, and no significant differences have been identified between these approaches.20,28
- According to the literature, it is recommended that reduction of the capitate precedes reduction of the scaphoid.
- Reduction of the scaphoid fragments is guided from the radial surface of the capitate and is not easily maintained if the capitate is not stabilized, as the proximal scaphoid fragment tends to displace into the gap of the capitate head.20
- Some authors recommended excision of the displaced proximal capitate fragment because of the possibility of avascular necrosis, but it’s been found that the capitate head can revascularize when replaced anatomically and immobilized until fracture healing.21
- Excision can also interfere with the function of the carpus and eventually result in osteoarthritis. It is therefore advised that the capitate fragment is not excised, even if it cannot be fixed.26
- Cancellous bone grafting may be considered in some cases of bone loss.20
Complications
- Infection
- Avascular necrosis
- Non-union
- Osteonecrosis
Outcomes
- Early surgical intervention with meticulous reduction and fixation of all fractures and dislocations present generally leads to a favorable result with minimal complications. Despite the severity of this injury, restoring normal anatomical relationships of the carpus can lead to a successful long-term functional outcome.20
- In one study of individuals with nondisplaced scaphoid fractures, those treated surgically returned to work earlier and had better functional outcomes than those treated conservatively.29
- Delayed diagnosis and treatment of this injury has been found to result in non-union with subsequent carpal arthritis and carpal collapse.26
Scaphoid dislocation and fracture-dislocation
- Scaphoid dislocation represents a wide spectrum of injuries with varying extent of ligamentous damage and may occur either in isolation or concomitantly with fracture(s) or other dislocation(s).
- In general, these injuries are rare, but isolated scaphoid dislocation without another associated fracture or dislocation is even more uncommon. This is because a substantial amount of force is required to disrupt the scaphoid from its fossa, and when this occurs, the radial styloid or scaphoid waist are typically also fractured.21,23,30
- A recent classification system has grouped isolated scaphoid dislocations into the following categories: primary or secondary, simple or complex, and partial or total.
- Primary dislocations result directly from the injury, while secondary dislocations persist after failed closed reduction.
- Simple dislocations involve only the scapholunate and radioscaphoid, while complex types have distal carpal row involvement.
-
-
-
- The exact mechanism of injury is not known, but it is generally believed that scaphoid dislocations are caused by violent dorsiflexion of the wrist with the hand grasping a fixed object in ulnar deviation. This provokes the disruption of the scaphoradial, scapholunate, and scaphohamate articulations, which causes the scaphoid to dislocate and often rotate out of its correct anatomical position while maintaining the integrity of the ligaments supporting the lunate, triquetrum, and hamate.21,23,30
- The severity of the injury is largely dependent on the number of ligaments disrupted, and it is postulated that the order of ligamentous failure begins with the radioscaphocapitate and scapholunate ligaments, followed by the radiolunate and scaphotrapezium-trapezoid ligaments.23,30
Imaging
- Standard radiographic views may not be sufficient to visualize an isolated scaphoid dislocation and the diagnosis may be occasionally missed.23
- To diagnose ligamentous injuries, it’s essential to identify the arcs of Gilula on plain radiographs. MRI and CT scan may also be needed to assess soft tissue damage.30
Treatment
- Treatment options for scaphoid dislocations and fracture-dislocations include closed reduction with cast immobilization, closed reduction and percutaneous pinning (CRPP) using K-wires, and ORIF with pinning and possible ligament repair.23
- One frequently cited management algorithm recommends the following:
- Closed reduction with cast immobilization for simple dislocations other than volar-ulnar that present <1 week from the traumatic event; however, reduction may be difficult to achieve through manipulation alone.
- Correct anatomic positioning of both the scapholunate articulation and angulation can be difficult, which necessitates conventional closed reduction methods with wire fixation.21,31
- For complex dislocations or when closed reduction fails and a secondary dislocation remains, ORIF is typically required.
- ORIF with K-wires is the most appropriate treatment option for secondary dislocations.
- ORIF with median nerve decompression is also advocated for simple dislocations with palmar-ulnar scaphoid displacement since the median nerve is usually found to be compressed in these patients.
- A volar approach allows better visualization of the scaphoid and provides better cosmetic results.21,23,30,31
Complications
- Avascular necrosis
- Posttraumatic osteoarthritis
- Carpal instability
- Infection
Outcomes
- When isolated scaphoid dislocations are treated early and appropriately, the prognosis is typically good, with complications being uncommon and most patients returning to their previous activities. Therefore, the most significant risk factor for poor prognosis is delayed diagnosis and treatment.21,23
Scaphoid avulsion fracture
- Most scaphoid avulsion fractures are distal pole and tubercle fractures that are believed to occur from direct impact and forced ulnar deviation of the wrist, which results in an avulsion at the radial collateral ligament attachments.
- The fragment may also be avulsed by the capsular attachments or the transverse carpal ligament.4,32
- None of the commonly used classifications of scaphoid fractures include the avulsion fracture pattern.32
- The smallest fragments identified on radiographs in one study were avulsion fractures from the tip of the tubercle.14
Imaging
- A 45° anteroposterior (AP) oblique—or “ball-catcher’s” view—is recommended for visualizing scaphoid avulsion fractures, and it may be the only way of distinguishing certain cases.32
- A semi-pronated view may also be helpful for assessing the scaphotrapezium-trapezoid joint.14
Treatment
- Scaphoid avulsion fractures are difficult to manage and there is no clear consensus on the optimal treatment for these injuries.32
- ORIF with K-wires has been suggested for displaced distal articular fractures of the scaphoid.14
Complications
Outcomes
- Isolated dorsal scaphoid avulsions appear to have a good prognosis and in themselves may not have major clinical significance; however, they may mimic scaphoid waist fractures, particularly those of the proximal pole, which have a significantly worse prognosis.32
Trans-scaphoid perilunate dislocation and fracture-dislocation
- Perilunate dislocations and fracture-dislocations comprise a spectrum of challenging injury patterns that can involve several carpal bones and their respective articulations. These injuries are generally considered rare and only account for ~10% of all carpal injuries33, and perilunate fracture-dislocations have been found to occur at about double the frequency of perilunate dislocations.25,34,35
- The trans-scaphoid perilunate fracture-dislocation is the most common injury pattern within this spectrum and has been reported to represent 61% of these injuries.35
- These injuries are produced by wrist hyperextension, usually in sports, a motor vehicle accident, or a fall from a height. This causes a disruption of the volar capsuloligamentous complex, starting radially and propagating through the carpus in an ulnar direction, then taking a transosseous route through the scaphoid.
- As opposed to purely ligamentous lesser arc injuries, the trans-scaphoid perilunate fracture-dislocation is a greater arc injury in which the fractured scaphoid is the initial destabilizing factor of the carpus. Other transosseous greater arc variants include fractures of the capitate, radial/ulnar styloid, or triquetrum, or combinations thereof.25,36
- The Mayfield et al. classification system for perilunate injuries and carpal instability is commonly used to better describe the sequence of injuries and to inform treatment decisions:
- Stage I: scapholunate dissociation, with failure of the scapholunate or radioscaphocapitate ligament
- Stage II: perilunate dislocation, in which the capitolunate joint is disrupted
- If the wrist is radially deviated in this stage, the force transmits through the scaphoid waist instead, resulting in a trans-scaphoid perilunate fracture dislocation.37
- Stage III: midcarpal dislocation, which includes disruption of the triquetrolunate interosseous ligament or triquetral fracture; neither the capitate or the lunate is aligned with the distal radius
- Stage IV: lunate dislocation from the lunate fossa, which usually occurs in a volar direction and involves a failure of the radiocarpal ligament38
- Stage V: complete volar lunate dislocation with a carpal fracture
- The most severe type of perilunate fracture-dislocation
- Added subsequently by Cooney et al.39
Imaging
- Diagnosis is difficult, and it’s been found that up to 25% of perilunate dislocations and fracture-dislocations are missed on clinical and radiographic examination. Failing to properly diagnose these injuries can lead to a delay in management and unfavorable outcomes.34,40
- Standard wrist posteroanterior (PA) and lateral radiographs are most useful.
- The PA view should be scrutinized for uneven gapping in the carpal bones, and the 3 smooth carpal arcs of Gilula should be free of discontinuity.34
- A CT scan may be needed if there is any doubt and in order to avoid a delay in diagnosis.
- Can determine the type of fracture(s), the amount of displacement, degree of comminution, if there are any associated ligament injuries, and to identify occult fractures.34,41
- MRI without contrast is effective for identifying intercarpal ligamentous ruptures and occult fractures or bone bruises. MRIs are therefore more useful for lesser arc injuries.34,42
Treatment
- Treatment options include closed reduction and cast immobilization, CRPP, and ORIF. Although there is still ongoing controversy regarding the optimal management protocol, in recent times a surgical approach has come to be generally favoured over solely closed methods.25,43
- This shift is partially attributed to CRPP being associated with unsatisfactory carpal alignment and poor functional outcomes. Closed reduction, however, is still the initial treatment-of-choice, but it’s only a temporizing treatment to prevent progression of median nerve neuropathy and must be followed by intercarpal fixation within the proximal carpal row, and ligamentous repair.25,37
- Reduction is performed with the elbow flexed to 90° and the hand placed into finger traps.
- Stable closed reduction is typically achieved, with reported maintenance of reduction in >90% of cases, and significant muscle relaxation improves the chances for a successful closed reduction.34
- After closed reduction, some surgeons perform immediate ORIF, while others prefer a period of cast immobilization before surgery.43
- The surgical maxim for greater arc injuries is fixation of the bony involvement before soft-tissue repair. Scaphoid fractures are typically fixed using cannulated headless screw systems, while comminuted fractures can be treated with K-wire fixation and autologous bone grafting from the distal radius.34
- Dorsal, volar, and combined approaches have been described, with advantages and disadvantages of each.
- A combined approach allows better visualization, but there is suspicion of increased risk of wound healing and other complications, while a dorsal approach allows good exposure of the proximal carpal row, midcarpal joints, and proximal pole of scaphoid. A volar approach is best suited for patients with suspected volar ligament injury and acute carpal tunnel syndrome.37
- The primary risks of ORIF are stiffness and injury to the joint capsule or ligamentous structures, while CRPP—which is highly associated with recurrent instability and carpal incongruity—may lead to more posttraumatic arthritis.43
- Salvage procedures such as wrist arthrodesis or proximal row carpectomy may be needed in cases of severely delayed diagnosis.25
Complications
- Carpal tunnel syndrome
- Posttraumatic osteoarthritis
- Median nerve dysfunction
- Complex regional pain syndrome
- Hand or wrist weakness
- Tendon ruptures/dysfunction
- Residual carpal instability
- Infection
- Malunion
- Non-union
- The risk of non-union is generally higher in perilunate fracture-dislocations due to increased soft tissue damage at the time of injury and the increased carpal instability thereafter.36
Outcomes
- The main factors that determine the clinical outcome in trans-scaphoid perilunate fracture-dislocations are time from injury to treatment, anatomic classification, and open or closed nature of the injury.25
- In general, non-union rates have been found to be higher in cases treated with closed reduction.25
- Although prompt surgical intervention can potentially avoid progressive carpal instability, it has been reported that over 50% of operatively managed patients can develop posttraumatic osteoarthritis.36
- However, conflicting this is one trial of 34 patients with perilunate dislocations, 23 of which had trans-scaphoid perilunate fracture dislocations. A total of 20 patients were treated surgically and 14 nonsurgically, and at follow-ups of >5 years, clinical and radiological outcomes were practically identical between groups. This suggests that surgery does not necessarily increase the rate of degenerative changes.43
- In one series of 18 patients with trans-scaphoid perilunate fracture-dislocations, 7 were managed surgically with a minimum 10 years follow-up.
- Three patients had an excellent or good Mayo wrist score, while 4 had radiographical evidence of degenerative changes at follow-up, but there was only 1 nonunion.44
Related Anatomy
- The scaphoid consists of a distal tubercle, a distal pole, a medial waist, and a proximal pole. It articulates distally with the trapezium and trapezoid, medially with the capitate, ulnarly with the lunate, and proximally with the radius at the scaphoid fossa. Derived from the Greek term “skaphe,” meaning skiff or boat, the scaphoid is approximately the size and shape of a medium cashew and is the largest and most radial of the proximal carpals, where it functions as a mechanical link between the proximal and distal carpal rows.
- Articular cartilage covers ~80% of the scaphoid’s surface and includes both the proximal and distal pole articulations. It also forms the radial border of the carpal tunnel.
- The scaphoid flexes with wrist flexion and radial deviation and extends during wrist extension and ulnar deviation.2,4
- Ligamentous attachments of the scaphoid include the radioscaphocapitate, long radiolunate, radioscapholunate, scapholunate interosseous, dorsal radiocarpal, dorsal intercarpal, scaphotrapezium-trapezoid, scaphocapitate, and transverse carpal ligaments. The existence of several other possible ligamentous attachments, including the radial collateral and volar scaphotriquetral ligaments, is still debated.45
- From an anatomical and biomechanical standpoint, the 3 major stabilizers are the scapholunate, radioscaphocapitate and long radiolunate ligaments.21
- The scaphoid has no tendinous attachments.
Incidence and Related injuries/conditions
- Fractures of the carpal bones have been found to account for between 8-18% of all hand fractures46,47 and ~6% of fractures overall.33
- Fractures of the proximal carpals are more common than the distal carpals, and the most commonly fractured carpal bone is the scaphoid, which represents 58-89% of all carpal fractures.46,47,49
- Fractures of the other 7 carpals are very rare and only account for ~1.1% of all fractures. The triquetrum is the most commonly involved of these bones, while fractures of the other carpals are even more rare and vary in incidence.50-52
- Scaphoid fractures comprise 2-7% of all orthopaedic fractures and are second only to the distal radius in most common wrist injuries.5,53,54
- The incidence of scaphoid fractures in the U.S. is estimated to be 10.6-29 per 100,000 person-years.55-57
- The male-to-female ratio for scaphoid fractures varies greatly from 2:1 to 13:1. These injuries can occur at any age but are most common in young men, with a peak incidence in the second and third decades—particularly ages 20-24—and are relatively rare in children and the elderly.3,49,57
- The high incidence in this demographic is likely due to participation in extreme and contact sports, and manual labor work, with athletes involved in football and basketball being especially prone.3
- One study reported that ~1% of college football athletes will sustain a scaphoid fracture.58
- According to one study, ~65% of scaphoid fractures occur in the waist, 15% in the proximal pole, 10% in the distal pole, and 8% in the tubercle, while fractures in the coronal plane are exceedingly rare.13