Fracture Nomenclature for Humeral Shaft fractures
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Humeral Shaft Fractures, the historical and specifically named fractures include:
Holstein-Lewis fracture
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Humeral shaft fractures are common injuries that most frequently occur in men aged 21–30 and women aged 60–80. In younger patients, these injuries usually occur due to a direct blow to the arm (e.g., car accidents, sports injuries), while in older patients, the mechanism of injury is a fall on an outstretched hand in which the humerus takes the brunt of the impact. Many patients with humeral shaft fractures have concomitant radial nerve injury due to the proximity of the nerve to the bone. Most humeral shaft fractures are amenable to conservative treatment consisting of immobilization and/or functional bracing, and positive outcomes are likely with this approach. Surgery may be indicated in patients with extensive concomitant injury and if conservative treatment fails.1-3
Definitions
- A humeral shaft fracture is a disruption of the mechanical integrity of the humeral shaft.
- A humeral shaft fracture produces a discontinuity in the humeral shaft contours that can be complete or incomplete.
- A humeral shaft fracture is caused by a direct force that exceeds the breaking point of the bone.
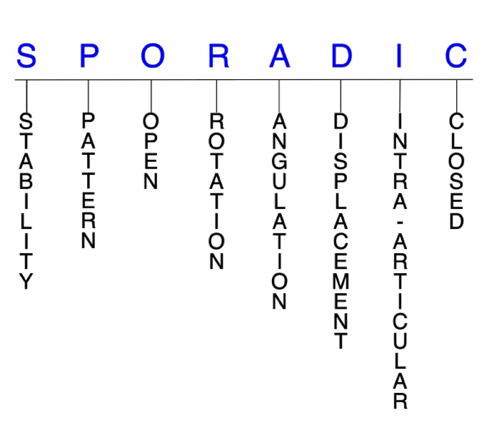
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability are not well defined in the literature.4-6
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragments’ alignment is maintained by with simple immobilization. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and immobilization. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Most humeral shaft fractures are unstable, but conservative management is still considered the gold standard in most cases.1
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and immobilization. Typical unstable humeral shaft fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
P - Pattern1,3
- Type A: simple fractures
- Type A1: spiral
- Type A2: oblique
- Type A3: transverse
- Type B: wedge fractures
- Type B1: spiral (intact)
- Type B2: bending (intact)
- Type B3: fragmented
- Type C: complex/multifragmentary fractures
- Type C1: spiral
- Type C2: segmental
- Type C3: irregular
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the humeral shaft require antibiotics with surgical irrigation and wound debridement.4,7,8
R - Rotation
- Humeral shaft fracture deformity can be caused rotation of the fracture proximal fragment in relation to the distal fracture fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angular deformity
- Angulated: bent at the fracture site
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: ≥1 fracture lines defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
- Holstein-Lewis fractures involve displacement of the distal fracture fragment and a simple spiral fracture pattern.2
I - Intra-articular involvement
- Intra-articular fractures are those that enter a joint with ≥1 of their fracture lines.
- Humeral shaft fractures can extend to have fragment involvement at the glenohumeral, ulnohumeral, or radiocapitellar joints.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to post-traumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised, and the risk of post-traumatic osteoarthritis increases significantly.
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.4-6
Humeral shaft fractures: named fractures, fractures with eponyms and other special fractures
Holstein-Lewis fracture
- The Holstein-Lewis fracture pattern is a simple spiral fracture of the distal humeral shaft in which the distal fragment is displaced, and the proximal end is deviated towards the radial side.2,9
- Concomitant radial nerve injury is common in Holstein-Lewis fractures because the distal fragment can potentially lacerate or entrap the radial nerve after it is displaced.2,9
- Holstein-Lewis fractures account for approximately 7.5% of all humeral shaft fractures and are more common in younger patients following high-energy trauma.2
Imaging
- Radiology studies - X-ray
- Radiographs are usually sufficient to diagnose these injuries.10
Treatment
- Although it was once believed that surgery was necessary for Holstein-Lewis fractures, most of these injuries are now treated nonsurgically. Conservative treatment includes immobilization using a coaptation splint with a collar and cuff or sling and swathe.10
Complications
- Radial nerve palsy
- Nonunion
- Stiffness
Outcomes
- According to one study, long-term outcomes were comparable between patients with Holstein-Lewis fractures who were treated conservatively and surgically.9
Related Anatomy2,3,11
- The humerus is a long bone that can be divided into a proximal end, a long shaft, and a distal end.
- The proximal end consists of an anatomic neck, the humeral head, the surgical neck, and the greater and lesser tuberosities at its proximal end. The humeral head humerus articulates with the glenoid fossa of the scapula to form the glenohumeral joint.
- The humeral shaft extends distally from the proximal border of the pectoralis major insertion to the supracondylar ridge. It is nearly cylindrical in its proximal half and then becomes flattened and triangular towards its distal end. It has 3 major surfaces: the anterolateral, anteromedial, and posterior surfaces.
- At the distal end, the medial condyle articulates with the ulna to form the ulnohumeral joint, and the capitellum articulates with the radial head to form the radiocapitellar joint.
- The humeral shaft serves as an insertion site for the pectoralis major, deltoid, and coracobrachialis tendons, and is the origin site for the brachialis, triceps, and brachioradialis tendons.
- Two important regions of the humeral shaft are the deltoid tuberosity and the radial groove.
- The deltoid tuberosity is an elevation near the middle of the anterolateral surface, which is the insertion point of the deltoid tendon.
- The radial groove or sulcus starts distal to the attachment of the lateral head of triceps on the posterior surface and runs distal and lateral toward the anterolateral surface. The radial nerve and profunda artery both pass within this groove.
- The radial nerve is the major nerve of the humeral shaft, which is located 14 cm proximal to the lateral epicondyle and 20 cm proximal to the medical epicondyle. Its proximity to the osseous anatomy of the humerus explains why the radial nerve is at such a high risk for injury in humeral shaft fractures.
Incidence
- Humeral shaft fractures account for about 1–3% of all fractures.12
- The incidence of humeral shaft fractures is approximately 13 per 100,000 persons per year, and about 66,000 humeral shaft fractures occur annually in the U.S.2,3
- The bimodal peaks for humeral shaft fractures are in men aged 21–30 years and women aged 60–80 years.1
- About 30% of humeral shaft fractures occur in the proximal third, 60% in the middle third, and 10% in the distal third of the bone.1