Fracture Nomenclature for Finger Middle Phalanx Fracture Pediatric
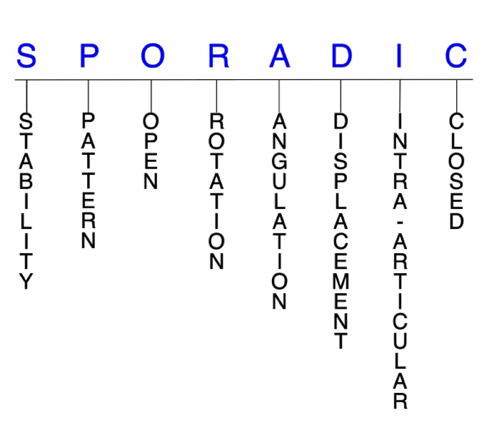
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Finger Middle Phalanx Pediatric, the historical and specifically named fractures include:
PIP joint volar plate avulsion fracture
PIP joint central slip avulsion fracture
Middle phalanx base epiphyseal fracture
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
The hand is the most common site of fracture in the pediatric population. The majority of these fractures occur in the phalanges, and the middle phalanx is least frequently affected of these bones, behind the distal and proximal phalanges, respectively. Mechanism of injury for pediatric middle phalanx fractures varies by age and includes falls, crushing forces, and sports participation. Although these fractures share some similarities with their counterparts in adults, special consideration must be given to key differences between the populations that will alter the diagnosis and management of middle phalanx fractures in children and adolescents.1-6
Definitions
- A pediatric middle phalanx fracture is a disruption of the mechanical integrity of the middle phalanx.
- A pediatric middle phalanx fracture produces a discontinuity in the middle phalanx contours that can be complete or incomplete.
- A pediatric middle phalanx fracture is caused by a direct force that exceeds the breaking point of the bone.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.7-9
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragments’ alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable pediatric middle phalanx fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
- In the pediatric population, even most displaced fractures are easily reduced closed and often quite stable.3
P - Pattern
- Middle phalanx head: oblique, transverse, or comminuted; can involve the distal interphalangeal (DIP) joint; these are intra-articular fractures that usually affect one or both condyles of the middle phalanx head with or without displacement; displaced fractures can affect joint congruity.
- Middle phalanx neck: fractures of the neck of the phalanges occur almost exclusively in children and are most common in the proximal phalanx, but can also occur in the middle phalanx; these fractures occur distal to the collateral ligament recess of the phalanx.1,3,10
- Middle phalanx shaft: transverse, oblique, or comminuted, with or without shortening.
- Middle phalanx base: can involve the proximal interphalangeal (PIP) joint; may be intra- or extra-articular and usually involve the dorsal or volar lip of the middle phalanx base;10 pediatric middle phalanx base fractures can also extend through the physis or metaphysis.1
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the pediatric middle phalanx require antibiotics with surgical irrigation and wound debridement.7,11,12
R - Rotation
- Pediatric middle phalanx fracture deformity can be caused by rotation of the distal fragment on the proximal fragment. Significant malrotation can affect the position of the fingertip during grip.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity; this is not a common type of fracture deformity in the pediatric middle phalanx.
- Radial or ulnar deviation and malrotation of pediatric middle phalanx neck fractures are also possible, and radiographs can underestimate the degree of clinical deformity.3
- Oblique fractures of the small finger are often malrotated, although physeal, transverse, intra-articular, and minor fractures by radiographic appearance can all be malrotated and lead to a rotated malunion.4
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- Example: pediatric middle phalanx neck fractures usually have apex volar angulation with associated sagittal and subcondylar malalignment.1
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: fracture line defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
- Most pediatric middle phalanx neck fractures are displaced, with dorsal translation and extension angulation.3
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- Pediatric middle phalanx fractures can have fragment involvement with the DIP or PIP joints.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
- Pediatric fractures of the middle phalangeal condyles are intra-articular and can involve one or both condyles. Fracture patterns include lateral avulsion fractures, unicondylar or intracondylar fractures, bicondylar or transcondylar fractures, and shearing fractures.3
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.7-9
Pediatric middle phalanx fractures: named fractures, fractures with eponyms and other special fractures
PIP joint volar plate avulsion fracture
- The common mechanism of injury is a “jammed finger” at the PIP joint secondary to a hyperextension force—such as in ball-handling sports like basketball and volleyball—which can result in an avulsion fracture of the volar surface of the middle phalanx epiphysis. 3,4,13
- The avulsion fracture size can range from a tiny flank to a larger fragment.10
- Volar plate avulsion fractures at the PIP joint are more common than central slip avulsion fractures.10
- Although not common, volar dislocation of the PIP joint may also be concomitant with these volar plate avulsion fractures.
- If a force is exerted on the middle phalanx from the dorsal to the volar side, the middle phalanx will dislocate to the volar side, and the lateral band can become interposed between the proximal and middle phalanges; this injury can also rupture the central slip when it crosses the dorsal head of the proximal phalanx.14
Imaging
- A true lateral X-ray view is essential to demonstrate if an avulsion fragment is present.
Treatment
- Despite the high incidence of these injuries in children and adolescents, specific treatment guidelines for the pediatric population are scarce.13
- Utilizing the most effective treatment protocol is therefore difficult, as there are several options available. Some physicians adopt protocols from adults to pediatrics, while others tend to follow general recommendations for fractures in children, particularly when a chip avulsion is visible in the radiograph.13
- Most PIP joint volar plate avulsion fractures should be treated with early motion after a short period of extension block splinting for up to 10 days. Bony union is never achieved, but a fibrous nonunion confers adequate joint stability.3,13
- Prolonged immobilization must be avoided in most cases because it can result in joint stiffness and permanent flexion contracture.13
- Some experts recommend early active mobilization with minimal or no splinting, but this has not yet been supported by the available evidence.13
- Certain cases of volar plate avulsion fracture with dislocation may be irreducible for several reasons, such as a longitudinal tear in the extensor tendon between the central slip and lateral bands or interposition of a collateral ligament or fracture fragment in the PIP joint. In children, the entire epiphysis may even be displaced and block reduction.15
Complications
- Swelling
- Boutonniere deformity
- Joint stiffness
- Permanent flexion contracture
Outcomes
- In one study, patients with stable volar plate avulsion fractures treated with dorsal extension block splinting for 10 days experienced positive outcomes with no need for subsequent supplementary immobilization at the follow-up.13
- Of the 33 patients with a complete follow-up, 31 (94%) had an excellent result and 2 (6%) had a good result.13
- This demonstrates that the extension block splinting intervention is effective and well tolerated, and results seemed to be superior to those in adults; however, questions remain as to whether these injuries can be treated in an even less invasive way and whether any treatment is needed at all.13
- Another study reported that stable PIP joint volar plate avulsion fractures were adequately managed with only minimal splinting or no treatment.16
- Central slip avulsion fractures at the PIP joint are rare compared to volar plate avulsion fractures, and it is important to differentiate the two injuries.3
- These types of avulsions result from hyperflexion, and similarly to volar plate avulsions, the most common injury mechanism is a jammed finger. This can tear the central slip from its insertion into the proximal portion of the middle phalanx.10
PIP joint central slip avulsion fracture
Typically, there is also injury to the extensor tendon that inserts into the middle phalanx, and a small avulsed bony fragment is often seen originating from the dorsal rim of the middle phalanx base.10
Imaging
- AP and lateral X-ray views are recommended.
- MRI and ultrasound may be needed to assess healing from these injuries if surgery is needed.
Treatment
- Small flecks avulsed from the dorsal rim of the middle phalanx can be treated like volar plate avulsion fractures as long as an Elson test indicates intact central slip function.3
- Larger, nondisplaced fragments should be treated with splint or cast immobilization to keep the PIP joint extended, thus allowing bony healing and restoration of the central slip insertion.
- Displaced fractures or those associated with PIP joint subluxation require open reduction and internal fixation (ORIF).3
- If the radial lateral band becomes interposed between the head of the proximal phalanx and base of the middle phalanx and the central slip ruptures, reduction is often needed.
- One method to accomplish this is to pull out the radial lateral band upward from the joint space by anchoring the ruptured central slip to the base of the middle phalanx and also repairing the collateral ligament.
- Three weeks of immobilization followed by active range of motion (ROM) exercises are recommended.14
Complications
- Swelling
- Stiffness
- Contracture
Outcomes
- Fixation of the central slip using the anchor system has been associated with good outcomes, but it is difficult to decide the most suitable anchoring position with a suture anchor since the original attachment of the central slip is on the epiphysis.14
Middle phalanx base epiphyseal fracture
- Epiphyseal fractures are prevalent in pediatric patients, and the phalangeal epiphyses are one of the most common locations for these injuries in children and adolescents.17
- Epiphyseal fractures of the middle phalanx base occur almost exclusively in elite adolescent sport climbers. The long and ring fingers are most commonly affected, and the fracture pattern is usually Salter-Harris type III.18
- These injuries typically result from excessive strain on the PIP joint, which is primarily a consequence of clinging to small handholds while climbing.18
- Salter-Harris type III fractures appear to be fatigue fractures caused by repetitive stress and microtrauma, and a possible injury mechanism is chronic microfractures of the dorsal part of the epiphysis.19
- Phalangeal epiphyseal fractures are becoming more common in skeletally immature patients as the sport of climbing is growing in popularity and young athletes are pushing their physical limits. It currently appears to be the most common injury among these athletes.18
- There is a greater risk of injury to the epiphysis when the growth plate cartilage is beginning to close in developing athletes.17
- The extensor mechanism of the PIP joint is attached by a median band to the dorsal articular capsule and is only attached to the middle phalanx at the epiphysis. Therefore, Salter-Harris type III fractures are also usually associated with injuries to the median band of the extensor mechanism.17
Imaging
- AP and lateral X-ray views
- Ultrasound
- MRI
Treatment
- Conservative treatment consisting of activity avoidance and gentle finger ROM exercises until fracture healing is recommended when a timely diagnosis is made and the fracture is nondisplaced, but surgery—such as ORIF—may be necessary when athletes present long after the initial injury with a displaced fracture and/or established nonunion.17,18
- A percutaneous spot drilling epiphysiodesis technique may be used for epiphyseal fracture nonunion, which is minimally invasive and easy to perform.18
- Extended activity avoidance may be sufficient for patients with Salter-Harris type II injuries.19
Complications
- Osteonecrosis
- Stiffness
- Angular deformity
Outcomes
- One study found that conservative management of nondisplaced middle phalanx base epiphyseal fractures was associated with excellent outcomes when the diagnosis was made early, but was more likely to fail in cases of delayed presentation, displaced fracture, and/or established nonunion.18
- Another study identified good outcomes with conservative treatment in patients who presented early, but worse outcomes with a longer interval between the onset of symptoms and the start of therapy. Researchers suggested that ORIF may therefore be needed in these patients.19
Related Anatomy
- The pediatric middle phalanx consists of a distal phalangeal head that articulates at the PIP joint with the distal phalanx, a supportive neck, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the PIP joint with the proximal phalanx. In developing children and adolescents, the physeal plate is located at the base of the middle phalanx, which has a dorsal and volar lip.1
- The ligaments associated with the middle phalanx at the DIP and PIP joints are the dorsal capsule, the proper and accessory collateral ligaments, and the volar plates, which stabilize the IP joints. The retinacular ligament, which runs obliquely along the middle phalanx, is also associated with this bone.
- Tendon attachments of the middle phalanx include the flexor digitorum superficialis tendon, which is inserted by two slips on either side of the base of the middle phalanx, and the extensor digitorum tendons. The central slip of the extensor tendon attaches at the dorsal epiphysis of the middle phalanx, and the terminal extensor tendon attaches at the dorsal epiphysis of the distal phalanx.1
- There is a basic anatomical difference between pediatric proximal and middle phalanges: the proximal phalanges have a longer, wider intramedullary canal with more cancellous bone, whereas the middle phalanges have a shorter, narrower intramedullary canal with more cortical bone. In general, fractures through cortical bone heal slower than fractures in cancellous bone.20
Incidence and Related injuries/conditions
- Metacarpal and phalangeal fractures account for 21% of all pediatric fractures, and the phalanges are the most commonly injured bones of the hands in this population.1,10
- The annual incidence of phalangeal fractures in children and adolescents up to 19 years old is approximately 2.7%.21
- Studies have shown that the proximal phalanx is the most frequently fractured phalangeal bone in the pediatric population, followed by the distal phalanx and the middle phalanx, respectively.5,6
- The incidence of phalangeal fractures is highest in children aged 10-14 years, which coincides with the time that most children begin playing contact sports. About two-thirds of these injuries occur in males, which is likely due to their participation in contact sports.1
- One study found that in the middle phalanx, fractures at the base of the bone were most common, followed by metaphyseal fractures.5
- Another study found that the older the child, the more proximal the fracture that was sustained, and despite more patients being right-hand dominant, the distribution of phalangeal fractures was similar in both the right and left hands.2